COVID-19 Situation Report
Editor: Alyson Browett, MPH
Contributors: Erin Fink, MS; Clint Haines, MS; Noelle Huhn, MSPH; Amanda Kobokovich, MPH; Aishwarya Nagar, MPH; Christina Potter, MSPH; Matthew Shearer, MPH; and Rachel A. Vahey, MHS

CALL FOR PAPERS Early detection of biological threats, whether naturally occurring or manmade, is critical. Threat agnostic approaches, which do not rely on determining the identity of the agent or pathogen, show early promise. In 2023, the Johns Hopkins Center for Health Security journal, Health Security, will issue a special feature that considers threat agnostic approaches to biodefense and public health. We encourage submissions of original research articles, case studies, and commentaries that explore policy gaps, data and data analysis, and implementation, among potential topics. The deadline is March 31, 2023. For more information, visit: https://www.centerforhealthsecurity.org/our-work/journal/call-for-papers/call-for-papers.html

EPI UPDATE* As of January 5, the WHO COVID-19 Dashboard reports:
- 657 million cumulative COVID-19 cases
- 6.67 million deaths
- 3 million cases reported week of December 26
- 22% decline in global weekly incidence as of December 26
- 10,794 deaths reported week of December 26
- 12% decline in global weekly mortality as of December 26
Over the previous week, incidence declined 73% in Africa; 42% in Europe; 26% in South-East Asia; 20% in the Americas; 16% in the Eastern Mediterranean; and 12% in the Western Pacific.
UNITED STATES
The US CDC is reporting:
- 100.6 million cumulative cases
- 1.09 million deaths
- 402,525 cases reported week of December 28
- 17% decline in weekly incidence as of December 28
- 2,530 deaths reported week of December 28
- 14% decline in weekly mortality as of December 28
- 17% increase in new hospital admissions
- 8.6% increase in current hospitalizations
*Recent holidays might delay data reporting for the WHO and US.
The Omicron sublineage XBB.1.5 experienced rapid growth over the past 2 weeks, accounting for an estimated 40.5% of all new sequenced specimens. BQ.1.1 (27%) and BQ.1 (18%) fall in line next, with various other Omicron subvariants accounting for the remainder of cases.
THE FOURTH YEAR As the COVID-19 pandemic enters its fourth year, many nations are better positioned to manage the disease due to clinical care management, vaccines, and therapies, WHO Director-General Dr. Tedros Adhanom Ghebreyesus said during a January 4 briefing. Nevertheless, inequities in access to testing, treatment, and vaccination remain, threatening individuals’ health, the global economy, and societies overall, he said, noting that approximately 10,000 people die of COVID-19 worldwide each week. On December 25, the WHO announced it prequalified the first generic version of Paxlovid for production by an Indian manufacturer and said its scientists are closely monitoring and evaluating the emergence of Omicron XBB.1.5, which is quickly spreading in the United States and has been detected in nearly 30 countries. WHO officials also expressed concern over the situation in China, urging health authorities there to regularly share reliable epidemiologic data.
OMICRON XBB.1.5 A new Omicron subvariant, XBB.1.5, has quickly become predominant in the United States, accounting for about 40% of all US cases—and 75% in the Northeast region—this week compared to around 4% of cases during the first week of December. XBB.1.5 is a recombinant Omicron sublineage, a fusion of 2 different BA.2 variants—BJ.1 (BA.2.10.1.1) and BA.2.75 (BA.2.75.3.1.1.1)—making it more closely related to the BA.2 subvariants that were predominant in the earlier part of 2022 than to the BA.5 subvariants that were responsible for most cases in the second half of 2022. Its rapid growth has concerned public health officials and healthcare practitioners alike, with WHO officials calling it the most transmissible subvariant detected yet. Though there is not yet much data on the severity of XBB.1.5, so far there is no indication it makes people more sick than previous subvariants. Hospitals in the US are already under significant stress, however, due to an early flu season as well as widespread incidence of other respiratory viruses such as RSV.
Some experts are concerned about XBB.1.5’s potential to evade prior immunity, with research on the related XBB subvariants showing the potential to escape the protections of antibodies resulting from vaccination, prior infection, or treatments, including Evusheld. In addition to being immune evasive, XBB.1.5 contains a mutation at genomic site 486 that is associated with enhanced viral binding to human ACE2 receptors, which could be boosting its transmissibility and causing it to surge. Notably, many experts highlight that vaccination and quick treatment with Paxlovid remains highly effective at preventing severe illness. It is unclear just how large of a surge may be driven by XBB.1.5, but the nation—and the world—is much better positioned at this point in the pandemic with vaccines, treatments, and nonpharmaceutical interventions such as masking helping to prevent infection, severe illness, and death.
US WINTER SURGE Much of the United States is experiencing a winter surge in COVID-19 cases, driven by waning immunity, holiday gatherings, and the emergence of the highly transmissible Omicron XBB.1.5 recombinant subvariant. Around the time of this report’s last publication on December 20, the nation surpassed 100 million cumulative reported COVID-19 cases, according to the US CDC. Federal data also show the number of hospitalized patients with COVID-19 is set to surpass the number reached during the summer 2022 surge, with new hospital admissions particularly high among individuals aged 70 and older who are most vulnerable to severe disease. Hospitals and clinics are feeling pressure from an influx of people with various respiratory illnesses in addition to COVID-19, including other coronaviruses that cause colds, influenza, and respiratory syncytial virus. Despite this, only 15% of people over age 5—and only 37.5% of those aged 65 and older—have received an updated bivalent vaccine booster dose. While recent data might not provide a clear picture of where the nation stands—due to reporting delays from recent holidays or severe weather as well as a lack of reporting from people using home tests—levels of SARS-CoV-2 detected in wastewater samples are rising in several regions, particularly in the Northeast, where the XBB.1.5 variant accounts for about 75% of new cases. Though health experts and some government officials, including those in New York City and Los Angeles, are urging people to begin wearing masks again and receive the latest booster, much of the country appears to have moved beyond the pandemic.
CHINA Following a reversal of its “zero COVID” containment strategy in early December after widespread protests, China is experiencing an unprecedented surge in cases. The outbreak appears to have spread first in urban areas, overwhelming healthcare facilities and morgues, and officials are concerned that weaker health systems in more rural areas will not fare well. The true impact of the current surge in cases and the number of resulting deaths is not fully understood due to unreliable data. The WHO has urged China to share more geographically based data on COVID-19 hospital admissions, intensive care unit (ICU) patients, and related deaths. Today, the organization said China supplied data on new COVID-19 hospitalizations showing a nearly 50% increase, from 15,161 new hospitalizations for mainland China during the week ending December 25 to 22,416 for the week ending January 1. China continues to report daily COVID deaths in single figures. The numbers likely are undercounts, based on officials’ use of a narrow definition of COVID-19 deaths, anecdotal evidence from individuals, and reports of deaths among prominent public figures.
In addition to the WHO, health and government officials worldwide are struggling to get a true sense of the situation in China and how to respond. Several countries have introduced—and the European Union recommended—pre-departure COVID-19 tests for travelers arriving from China, moves that the Chinese government and others have criticized as useless or even harmful. Some officials are concerned the large outbreak could provide an opportunity for a new SARS-CoV-2 variant to emerge. According to data from China’s CDC, the Omicron variant—specifically sublineages BA.5.2 and BF.7—is the most dominant based on recent genomic sequencing. The data allay concerns, for now, about the potential for a new variant of concern emerging from the outbreak, but some experts say the situation highlights the need to develop an early warning surveillance system using viral genomic data.
THERAPEUTICS Over the past several years, monoclonal antibodies were critical therapies for millions of people who were at high risk of getting sick from COVID-19 but who did not respond to or could not receive SARS-CoV-2 vaccines. However, new immune-evasive Omicron subvariants have rendered them largely ineffective as treatments for currently circulating SARS-CoV-2 variants, and even prophylactic antibody therapies like Evusheld show diminished efficacy. In 2022, the US FDA rescinded emergency use authorizations for major monoclonal antibody treatments including bamlanivimab, etesevimab, sotrovimab, casirivimab, imdevimab, and bebtelovimab, leaving immunocompromised individuals without many treatment options.
Other therapies have mixed benefits for immunocompromised individuals. Although antivirals are available,they have seen lackluster uptake and are not accessible to everyone; Pfizer’s Paxlovid interacts with other widely prescribed drugs, Merck’s Lagevrio shows lower efficacy, and Gilead’s intravenous remdesivir requires infusions over 3 days in hospital or outpatient settings. Although the US government has strongly promoted antivirals like Paxlovid,misinformation and misconceptions about the drug, as well as worries about side effects and viral rebounding after finishing a regimen, have hampered its uptake. Even convalescent plasma, which can be adapted to different strains,is inconsistently available and difficult to administer.
An FDA spokesperson said the agency will work with pharmaceutical companies on expediting the development of preventive therapies for immunocompromised patients, though it is unknown if the agency will accept fact-tracked data gathered from laboratory studies instead of large-scale clinical trials. Additionally, without the support of federal funding that drove drug development during earlier stages of the pandemic,pharmaceutical companies have little incentive to work on new and more effective antibody treatments. The lack of effective, specialized, and widely used therapies leaves many immunocompromised people with limited options if they become sick with COVID-19.
UNFOUNDED VACCINE RUMORS During a primetime US National Football League (NFL) game on January 2, Buffalo Bills player Damar Hamlin collapsed shortly after suffering a blow to his chest and subsequent cardiac arrest. Hamlin was resuscitated on the field and remains in critical condition in a Cincinnati hospital. Although little is known about the true cause of Hamlin’s collapse, cardiologistssuspect that the blow to his chest may have disrupted his heart’s rhythm and hindered blood flow to his brain; they note there is no indication Hamlin’s COVID-19 vaccine status played a role. Shortly after the incident, however, unfounded rumors began circulating on social media linking Hamlin’s injury to COVID-19 vaccines, revealing the pervasiveness of false and misleading information 3 years into the pandemic. The November 2022 rollback of Twitter’s ban on COVID-19 misinformation likely helped the rumors spread quickly and widely.
Although certain viral infections and vaccinescan lead to myocarditis in some instances, the risk ofvaccine-induced cardiac arrest associated with COVID-19 vaccines is inflated. A September 2022 study in the journalCirculation found that the risk of developing myocarditis following a booster dose of the Pfizer-BioNTech vaccine is low, and an August 2022 study published in Frontiers in Cardiovascular Medicine found that the risk of myocarditis is more than 7-fold higher in persons who were infected with SARS-CoV-2 than in those who were vaccinated. Additionally, a July 2020 study in theClinical Journal of Sport Medicine found that structural abnormalities of the heart muscle or arteries and faulty electric rhythms were the most common causes of sudden cardiac events among competitive professional athletes in the US.
With skepticism surrounding COVID-19 vaccines now threatening other public health priorities, including childhood vaccinations, health officials are struggling to combat misinformation and improve communities’ trust in public health. Experts are concerned that this new wave of misleading information surrounding COVID-19 vaccines threatens the rollout of updated booster doses and ongoing efforts to stop the spread of COVID-19 and other diseases such as measles.
MSNBCMcCarthy appears to lose seventh vote for speaker
NBC NewsMcCarthy appears to lose eighth vote for speaker
The Washington PostMcCarthy loses fourth vote for speaker






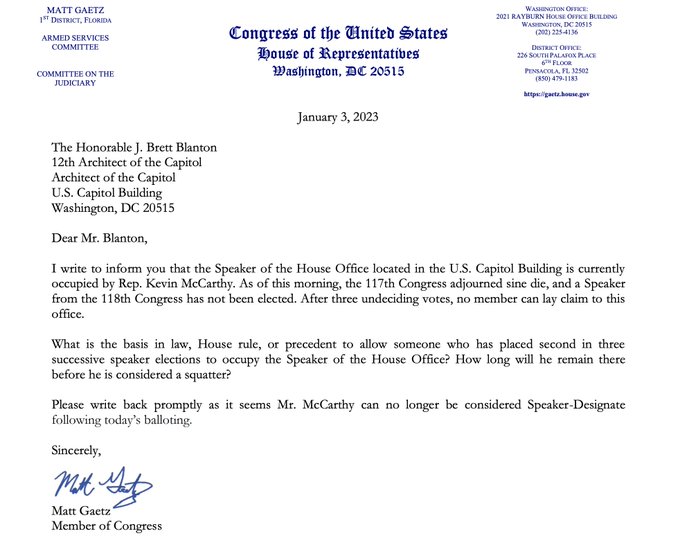



 NewsweekBoebert Calls For McCarthy To Withdraw As Trump Backs Him For House Speaker
NewsweekBoebert Calls For McCarthy To Withdraw As Trump Backs Him For House Speaker

 DailymotionLauren Boebert says Trump should tell McCarthy not to run for House speaker
DailymotionLauren Boebert says Trump should tell McCarthy not to run for House speaker