![]()
![]()
COVID-19
Updates on the COVID-19 pandemic from the Johns Hopkins Center for Health Security.
Additional resources are available on our website.
The Johns Hopkins Center for Health Security also produces US Travel Industry and Retail Supply Chain Updates that provide a summary of major issues and events impacting the US travel industry and retail supply chain. You can access them here.
![]()
EPI UPDATE The WHO COVID-19 Dashboard reports 67.21 million cases and 1.54 million deaths as of 11:00am EST on December 8. The global mortality surpassed 1.5 million deaths on December 4. The weekly incidence remained essentially the same as the previous week, and the global mortality continued to climb for the seventh consecutive week, an increase of 3.6% compared to the previous week.
UNITED STATES
The US CDC reported 14.64 million total cases and 281,253 deaths. The US reported 219,187 new cases on December 3, making it the first country to exceed 200,000 cases in a single day. After reporting more than 200,000 cases for the first time, the US exceeded 200,000 cases for 3 consecutive days—December 3-5. The US is currently averaging more than 190,000 cases per day. The US now ranks #11 globally in terms of per capita daily incidence, with 608 daily cases per million population. Of the 10 countries ahead of the US, 5 have populations of less than 1 million, and only Serbia (6.8 million) has a population greater than 5 million. Five (5) of those countries are averaging fewer than 600 total cases per day, and none are reporting more than 7,500.
Also on December 3, the US surpassed 14 million cumulative cases. From the first case reported in the US on January 22, it took 96 days to reach 1 million cases. From there:
1 to 2 million- 44 days
2 to 3 million- 27 days
3 to 4 million- 15 days
4 to 5 million- 17 days
5 to 6 million- 22 days
6 to 7 million- 25 days
7 to 8 million- 21 days
8 to 9 million- 14 days
9 to 10 million- 10 days
10 to 11 million- 7 days
11 to 12 million- 5 days
12 to 13 million- 7 days
13 to 14 million- 5 days
The US surpassed 275,000 cumulative deaths on December 3 as well. From the first death reported on February 29, it took 46 days to surpass 25,000 deaths. From there:
25k to 50k- 9 days
50k to 75k- 13 days
75k to 100k- 20 days
100k to 125k- 31 days
125k to 150k- 32 days
150k to 175k- 24 days
175k to 200k- 31 days
200k to 225k- 34 days
225k to 250k- 24 days
250k to 275k- 14 days
From December 1-5, the US reported more than 2,300 deaths for 5 consecutive days for the first time ever, including 2,861 deaths on December 3, the third-highest daily total to date. The US is currently averaging 2,171 deaths per day, the highest since April 25. This corresponds to 1.5 deaths every minute, or 1 death every 40 seconds. The US has only exceeded the current daily mortality for an 11-day period from April 15-25, at the peak of the first surge.
As a reminder, the CDC data from last week included delayed cases and deaths from over the Thanksgiving holiday weekend, which could have resulted in elevated figures over the past week. We expect that health departments and hospitals are caught up in their reporting, so this week will likely provide a more accurate representation of the current state of the US epidemic. It will still be at least another week before we could begin to see any effects on incidence stemming from Thanksgiving travel and gatherings.
The Johns Hopkins CSSE dashboard reported 14.98 million US cases and 284,131 deaths as of 11:30am EST on December 8.
UK VACCINATION The UK initiated SARS-CoV-2 mass vaccination today. Last week, the UK issued an emergency authorization for the Pfizer/BioNTech vaccine, and the initial supply of vaccines will include enough for 400,000 individuals at 2 doses per person. The UK’s vaccination priority groups list residents of long-term care facilities in the first tier of the initial phase, followed by individuals aged 80 years and older and frontline healthcare and social workers in the second tier. The actual operationalization of the earliest stage of the vaccination program, however, appears to be adapting that order to some degree. UK SARS-CoV-2 vaccination guidance indicates that vaccinations are currently only being administered at some hospitals—presumably due to the complex transportation and storage requirements to maintain the ultra-cold temperature needed to keep the vaccine viable—and that vaccination is currently limited to individuals aged 80 years and older who are hospitalized or already have a hospital appointment scheduled, long-term care facility staff, and high-risk healthcare workers. The guidance does indicate that availability and locations will be expanded “as soon as possible,” dependent on vaccine supply and the conversion and operation of suitable vaccine clinic sites. Vaccinations will be provided free of charge to everyone. As the first vaccination campaign among Western countries, the world will be watching closely to glean any lessons from the UK experience.
RUSSIA VACCINATION In addition to the UK, Russia reportedly opened vaccination to high-risk groups in Moscow earlier this week, including essential workers and those at elevated risk for severe disease and death. The vaccines are being administered at 70 clinics across Moscow, and Russian officials have stated that they expect to produce 2 million doses by the end of 2020, enough to cover 1 million people. Russia’s vaccination program is using its own Sputnik V vaccine, which has been authorized by the Russian government but has not yet completed Phase 3 clinical trials. The Russian government has reported that the vaccine is 92% efficacious; however, to our knowledge, supporting data have not been published publicly or subjected to peer review.
INDONESIA VACCINATION Indonesia reportedly received as many as 1.2 million SARS-CoV-2 vaccine doses from Chinese vaccine manufacturer Sinovac, and it expects to receive another delivery of 1.8 million doses in January. In addition to the direct delivery of vaccine doses, Sinovac is also planning to ship the raw materials required to produce the vaccine, which will enable Indonesia to manufacture as many as 45 million doses domestically. Indonesian President Joko Widodo indicated that Indonesia is evaluating the vaccine for emergency authorization, and it aims to initiate vaccination before the end of the year. Indonesia’s state-owned pharmaceutical manufacturer, Bio Farma, reportedly issued a statement today that the Sinovac vaccine was demonstrated to have 97% efficacy in clinical trials; however, it later retracted the statement and noted that additional investigation was required. Sinovac previously announced that its vaccine generated an immune response in 97% of study participants; however, this was based on limited data from Phase 1/2 clinical trials rather than larger Phase 3 trials. Phase 3 clinical trials for the Sinovac vaccine are still in progress.
US FDA VACCINE EVALUATION The US FDA is in the process of reviewing Pfizer and BioNTech’s candidate SARS-CoV-2, after all necessary EUA paperwork was submitted on November 20. Following the UK’s emergency authorization of the vaccine last week, many in the US are hopeful that the FDA will quickly follow suit. The FDA maintains that it is working at full speed to accurately and carefully evaluate the vaccine candidate’s efficacy and safety, even as data from Phase 3 trials are still being collected. One of the most notable differences between the UK and US regulatory review is that the UK performed a “rolling review.” The UK’s process enabled regulatory officials to view trial data as they were collected, which shortened the final review once the final data were presented. Conversely, the US FDA waited until all data were collected in order to review it all at once, which is taking longer to complete.
In an upcoming meeting on December 10, the Vaccines and Related Biological Products Advisory Committee Meeting will review the Pfizer-BioNTech data and make recommendations to the FDA on whether the vaccine may be effective in preventing COVID-19 and whether its known benefits outweigh potential risks. While the VRBPAC’s recommendations will factor heavily into the FDA’s decision, the EUA authorization will remain solely in the hands of the FDA. This meeting will be streamed live on multiple platforms.
While the Pfizer/BioNTech candidate is intended to be administered as 2 doses, data published in advance of the December 10 meeting indicate that the vaccine can provide some measure of protection after the first dose. The data come from Phase 3 clinical trials, and they suggest that immunity begins to increase as early as 10 days after the first injection and that a single dose could have 52% efficacy. Although individuals will still need to return for a second dose to reap the full protective benefits, any protection conferred after the first dose would be a major advantage for this vaccine. It is possible that an EUA could be issued as early as the end of this week, and vaccination could begin within days of the announcement.
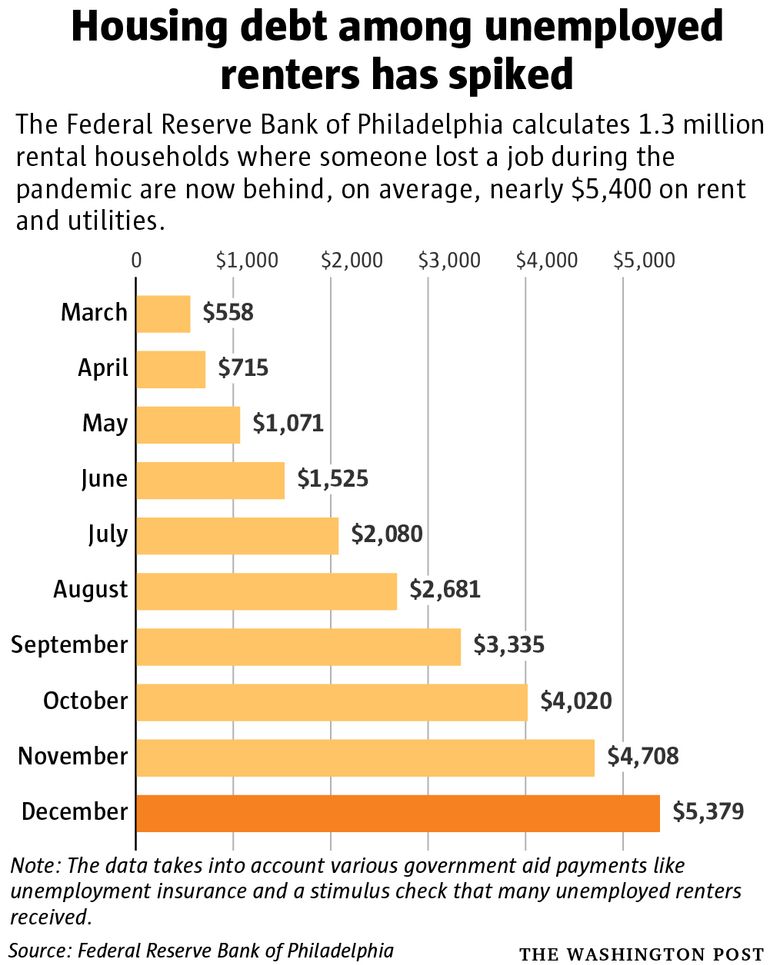
US ECONOMIC STIMULUS The US Congress continues to negotiate details of prospective COVID-19 economic stimulus packages, with the goal of providing major financial support for individuals and businesses for the first time since the CARES Act was passed in March. A bipartisan stimulus plan totaling more than US$900 billion is reportedly gaining some traction, although the overall plan was reportedly dismissed last week by Senate Majority Leader Mitch McConnell. Negotiations on COVID-19 funding are now interwoven with those for a federal government funding bill, adding further complexity to these discussions. Reportedly, the Congress is expected to pass a 1-week continuing resolution to stave off a federal government shutdown and provide extra time to finalize the details of a COVID-19 economic stimulus package that would be attached to the federal funding bill. Clearly, the details still need to be worked out, but high-profile issues include direct stimulus payments to individuals, funding for small businesses, and expanded unemployment insurance payments. Without additional funding, some portions of the CARES Act, including expanded federal unemployment insurance payments for 12 million people, will expire on Christmas 26, the day after Christmas. Some economists argue that the US would need an economic stimulus package of US$3-4.5 trillion in order to drive optimum economic recovery in the short term.
Today, Japan announced its own economic stimulus package to support recovery from COVID-19, totaling more than US$700 billion. The Japanese plan includes funding for longer-term investments, including in “green and digital innovation,” rather than focusing solely on the current direct impact of the pandemic. On a per capita basis, however, this would be approximately twice the investment as the proposed US economic package.
US HOSPITALIZATIONS The US Department of Health and Human Services (HHS) published detailed, facility-level data on hospital capacity with respect to COVID-19. The data cover more than 2,000 hospitals nationwide, and initial analysis by COVID Tracking Project found that 126 counties are reporting bed availability at 10% or less, principally in Kentucky, Georgia, Minnesota, Oklahoma, and Texas. The release of local data provides a much more detailed look at COVID-19 hotspots than the state-level hospitalization data previously available.
Over the past several weeks, the US has exhibited a dramatic increase in hospitalizations, in addition to incidence and mortality. According to data published by the COVID Tracking Project, the US surpassed 100,000 current COVID-19 hospitalizations on December 2, more than 40% higher than either of the first 2 peaks. Additionally, 34 states are reporting increasing COVID-19 hospitalizations (10% increase or greater) over the past 2 weeks. News media reports of overwhelmed hospitals continue to emerge across the country, and healthcare workers, health officials, and other experts continue to call on state and federal government officials to provide additional support, including enhanced social distancing measures and mask mandates to reduce community transmission. Beyond patient capacity limitations, many healthcare workers are struggling with exhaustion, as they never had the opportunity to recover physically, mentally, or emotionally from previous surges. Even if beds are available for new COVID-19 patients, hospitals need trained, qualified personnel to provide care, particularly for complex procedures like mechanical ventilation. If personnel are not available or are overwhelmed, patients may not be able to receive the level of care they need.
METFORMIN Diabetes is already recognized as an underlying condition that elevates the risk of severe COVID-19 disease or death. Past studies have indicated that glycaemic control, particularly via administration of anti-hyperglycemic drugs, can reduce this risk for COVID-19 patients with diabetes, although this relationship is not fully understood. A new study published in Lancet: Healthy Longevity found that use of metformin—a low-cost and safe generic drug used to treat type 2 diabetes—was associated with decreased COVID-19 mortality among women with type 2 diabetes or obesity. The researchers posit that this association was observed in women and not men as a result of the increased effect of metformin in lowering tumor necrosis factor ⍺ (TNF⍺) in women than in men, potentially supported by modulation of the ACE2 receptor, decreased inflammatory cytokine response, and other factors. They also note that since 42% of women in the US have obesity, these findings could have a major impact on the severity of the US COVID-19 epidemic. Further study regarding preventative use of metformin and the causative mechanisms behind its effect on COVID-19 mortality are needed to better characterize the treatment effect of metformin, but this study does provide additional information that could mitigate the risk of severe disease and death among high-risk patients who have obesity or type 2 diabetes.
In an accompanying commentary, two researchers from the University of Pisa (Italy) caution that these early findings could be driven by a number of potential confounding factors in the study. In particular, the authors note that the retrospective study design could lead to inherent biases related to patient inclusion and that the study populations had lower prevalence of other underlying health conditions than the broader population, including coronary artery disease, heart failure, chronic kidney disease, and end-stage renal disease. Additionally, as with many studies conducted during the pandemic, differences in the standard of care across multiple healthcare facilities could impact the study findings.
LONG-HAULERS Last week, the NIAD hosted its first workshop on long-term health effects of COVID-19. The event included input from public health experts, medical researchers, government officials, and patients. There is currently no definitive estimate of how many people suffer these long-term cardiac, neurological, respiratory, or other effects following recovery from SARS-CoV-2 infection—commonly referred to as “long haulers”—but it is clear that long-term COVID-19 sequelae will become a major public health problem, if even only a small fraction of individuals are affected. To address this threat, workshop attendees recommended that the syndrome be assigned an official, distinct medical term in order to increase awareness and prompt investigations necessary to more fully characterize the phenomenon.
AFRICA INFODEMIC RESPONSE ALLIANCE Last week, the WHO announced a new initiative to fight COVID-19 misinformation in Africa as well as during future health emergencies. The new Africa Infodemic Response Alliance will bring together 13 international and regional, including fact-checking groups, to “detect, disrupt and counter damaging misinformation on public health issues in Africa” and to promote the sharing of scientifically accurate information by journalists and news media, utilizing guidance developed by the WHO’s Information Network for Epidemics (EPI-WIN). Participating members and bodies include the Africa Centres for Disease Control and Prevention, International Federation of the Red Cross and Red Crescent Societies, UN Verified initiative, UN Children’s Fund (UNICEF), UN Educational, Scientific and Cultural Organization, UN Global Pulse, Africa Check, Agence France-Presse Fact Check, PesaCheck, Dubawa, and Meedan.
WORKER SAFETY The safety of frontline and essential workers, particularly those with roles that cannot be performed remotely remains a major area of concern for employers and policymakers. At the federal level, the US Occupational Safety and Health Administration (OSHA) is tasked with setting national standards for workplace safety across all industries; however is has been criticized on multiple fronts for not taking sufficient action to protect worker safety during the COVID-19 pandemic. While OSHA has the ability to raise standards for occupational safety, a federal appeals court recently sided with OSHA’s stance that an emergency temporary standard was not necessary. Since then, many state and local governments implemented their own temporary workplace standards that include enhanced measures beyond those required by OSHA. State-imposed requirements include improved indoor ventilation, increased physical distancing between employees, and routine diagnostic testing. This state-by-state approach to worker safety has created a patchwork of regulations across the US, potentially leading to unequal burden of disease, even among workers in the same industry or company, depending on where they live. Many experts are calling on President-Elect Joe Biden to create uniform, national occupational safety standards when he takes office in January. While states could still choose to enact more restrictive measures on top of a national standard, raising the baseline level of protection for workers could simplify workplace safety and increase equity nationally.
WHO SOLIDARITY TRIALS The WHO Solidarity Trial Consortium published the interim results from its clinical trials of remdesivir, hydroxychloroquine, lopinavir, and interferon beta-1a in The New England Journal of Medicine. The results were published previously as a preprint version, but the new publication has been subjected to peer review, with associated edits incorporated. Some of the language and numbers have been updated, but the overall findings remain essentially the same. Most notably, the 4 candidate treatments were found to have “little or no effect on hospitalized patients with Covid-19” including on “overall mortality, initiation of ventilation, and duration of hospital stay.” The one exception is remdesivir, which did demonstrate a “small effect” in terms of improving recovery time, as has been demonstrated in other clinical trials; however, it did not improve overall mortality.
The peer reviewed publication was accompanied by an editorial by researchers at Harvard and Brown Universities (US) that highlighted the Solidarity Trial’s achievements. The authors applaud the research effort, which established and implemented a common randomized clinical trial protocol involving more than 11,000 patients across 405 hospitals in 30 countries. The relatively simplified trial design, including “easily measured definitive outcomes that can be collected quickly and accurately,” enabled it to be implemented at facilities in all 6 WHO regions, representing a variety of healthcare settings, which allowed the trials to account for a broad spectrum of standards of clinical care as well. The authors argue that the mixed results for remdesivir—ie, that it could speed recovery in some hospitalized patients but not necessarily reduce mortality—will require “placebo-controlled trials with complex data.” A trial design capable of providing more nuanced findings on the role of remdesivir as a COVID-19 treatment likely would have been difficult or impossible to implement on such a large scale, across healthcare facilities with such a wide scope of resources and capabilities. Overall, the Solidarity Trial provided critical information on multiple candidate treatments in a relatively short period of time.