![]()
![]()
COVID-19 Situation Report
![]()
Editor: Alyson Browett, MPH
Contributors: Clint Haines, MS; Natasha Kaushal, MSPH; Amanda Kobokovich, MPH; Christina Potter, MSPH; Matthew Shearer, MPH; Marc Trotochaud, MSPH; and, Rachel A. Vahey, MHS.
![]()
RISE OF OMICRON The Omicron variant of concern (VOC) has become the predominant variant across North America and Europe, while the rest of the world braces for the eventual takeover. The WHO announced on December 18 that 89 countries have now reported Omicron within their borders, with high likelihood that cases are in many other countries but have simply not yet been confirmed. While the Delta VOC previously overtook other circulating variants to become the predominant SARS-CoV-2 variant, Omicron’s rise in these regions occurred precipitously, within 1 month after it was first reported in South Africa on November 24. While preliminary data out of South Africa indicated that infection with the Omicron variant was less likely to lead to hospitalization, the sheer number of cases resulting from the highly transmissible variant appear to be causing significant healthcare strain and societal disruption.
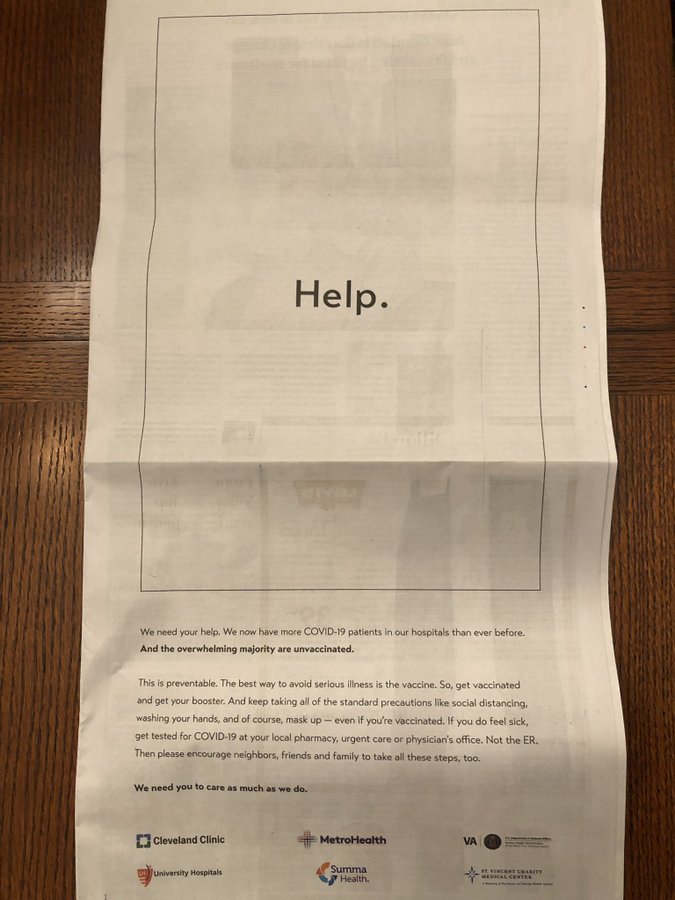
In the US, Omicron now accounts for 73.2% of the total number of SARS-CoV-2 infections, compared to 1 week ago when it accounted for only 12.6% of all infections. As of December 20, 48 states, Puerto Rico, and Washington, DC, have reported cases of Omicron; South Dakota and Oklahoma have yet to report cases. This rapid increase in Omicron cases has startled public health officials. With cases currently doubling every 1.5 to 3 days, healthcare facilities are bracing for a surge in hospitalizations, with some regions already experiencing these challenges. In the Northeast, where cases are currently surging, states like Rhode Island and Maine are reporting that their hospitals are being strained to their limits. As community members seek medical care in high numbers, healthcare staff are also testing positive for SARS-CoV-2, further exacerbating the strain on resources. Some states are activating their National Guards to help bolster medical, testing, and vaccination efforts. With testing lines wrapping around city blocks and holiday travel quickly approaching, public health officials are urging all who are able to get fully vaccinated and receive their booster shots. US President Joe Biden is set to address the nation tonight and is expected to announce plans to supply free tests and more aid for hospitals.
Outside of the US, other countries are facing the same challenges with the added difficulties of lower vaccination rates due to decreased access and supply. While most world leaders seem hesitant to initiate lockdowns akin to the initial March 2020 responses, many are implementing restrictions in an effort to slow the entry of Omicron into their nations. Israel has banned travel to North America and many European countries, while Asia Pacific island nations are moving to close their borders to international travelers or at least increase surveillance and quarantine measures for inbound travelers. In many European countries where Omicron is already spreading at high rates, some leaders are considering implementing stricter measures ahead of the holiday season. In the UK, Prime Minister Boris Johnson stated he is considering a number of measures, including lockdowns, as COVID-related hospitalizations rise. Regardless of strategy, all countries are trying to accelerate their vaccination programs to prevent a collapse of their healthcare systems.
VACCINE EFFICACY As the Omicron variant of concern (VOC) continues to rapidly spread around the world, preliminary data all of the vaccines appear to provide protection against severe disease, but most of the SARS-CoV-2 vaccines used worldwide may offer little defense against infection from the highly contagious variant. According to a not-yet-peer-reviewed analysis from Imperial College London, Omicron can largely evade vaccine-induced immunity or immunity from a past infection, with the risk of reinfection estimated to be 5.4 times greater than that with the Delta VOC. The researchers estimated that vaccine effectiveness (for AstraZeneca-Oxford and Pfizer-BioNTech vaccines) against symptomatic Omicron infection is between 0% and 20% after 2 doses and between 55% and 80% after a booster dose. Preliminary laboratory results from Moderna released this week in a press release showed a 50 μg booster dose—the same formulation authorized as a booster by the US FDA—produced a 37-fold increase in neutralizing antibodies compared with the primary 2-dose series, while a full 100 μg dose booster produced an 83-fold increase over 2 doses. The full dose had slightly more side effects than the half dose. Pfizer-BioNTech earlier this month announced a booster dose of their vaccine also helped increase neutralizing antibodies against Omicron. All of the studies are preliminary and do not take into account the full spectrum of the human immune response.
Still, some experts are saying that a 3-dose vaccination schedule will be necessary and some evidence shows the time between a second and third dose can be shortened from 6 months to 3 months. Several countries—such as South Korea, UK, Thailand, Belgium, France, Singapore, Taiwan, Italy, and Australia—have decreased the required wait time between doses to between 3 and 5 months to prepare for the arrival of Omicron. Others—including the US, South Africa, and Germany—are sticking to a 6-month schedule. Though there is some concern that shortening the gap could compromise immune response to vaccinations, others say a 6-month interval is arbitrary and urge booster doses sooner to counter waning antibody levels. Many uncertainties remain about how pre-existing immunity, whether from vaccination or previous infection, will help during infection with Omicron, and some evidence suggests Omicron-specific vaccine boosters will be necessary. While many higher-income nations are focused on vaccinating, and boosting, their populations, only 8% of the populations in low-income countries have received at least 1 dose of vaccine. It is important that the international community not lose focus on global goals pertaining to vaccine access and administration.
OMICRON SEVERITY An initial study (unpublished) on the severity of the SARS-CoV-2 Omicron variant of concern (VOC) conducted in South Africa suggests that adults are approximately 30% less likely to be hospitalized due to severe COVID-19 now than during the Delta surge. Health experts from the region also claim that hospitalized patients are less likely to end up on ventilators or require intensive care, on average, than during previous surges of COVID-19. However, scientists and public health officials have been quick to point out that the mild reactions to Omicron in South Africa may not be seen in Europe and the US. A large percentage of the South African population is young, by comparison, and many already have some immunity to SARS-CoV-2 due to prior infection during previous surges or vaccination. This immunity is believed to be a prominent factor driving the reduced disease severity observed in South Africa. In the US, researchers from the Covid-19 Modeling Consortium at the University of Texas at Austin looked at 18 different scenarios for Omicron, warning that under the most pessimistic model, “Omicron could lead to the largest healthcare surge to date, unless measures are taken to slow spread.” The data have not yet been peer-reviewed.
As such, concerns over hospital capacity are rising, as many individuals are expected to travel and spend time with family during the holiday season, increasing the risk of transmission of the highly contagious VOC. US states such as New York and New Jersey are already reporting high hospitalization rates and an increased demand for testing. The US Department of Health and Human Services (HHS) reports that more than 76% of ICU beds are currently in use, with 21% of those beds being used for COVID-19 patients. Additionally, Regeneron and Eli Lilly are warning that their antibody treatments for COVID-19 might be less potent against Omicron. The US reported its first Omicron-related death on December 20. The UK offers an unsettling potential lens into the future for the US. The UK Health Security Agency reports at least 14 deaths due to Omicron and 129 hospitalizations as of December 20, up from 7 and 85 on December 18. While it remains too early to tell the damage Omicron will inflict, the growing number of deaths and hospitalizations indicate that the variant should not be viewed as a slightly worse form of the common cold.
NOVAVAX VACCINE Following months of manufacturing delays, the 2-dose SARS-CoV-2 vaccine from biotechnology company Novavax, NVX-CoV2373, received conditional marketing authorization by the European Commission on December 20 and an emergency use listing (EUL) from the WHO on December 17. In Europe, the vaccine is known as Nuvaxovid and is the fifth vaccine to receive authorization to prevent COVID-19 in adults aged 18 years and older. Novavax expects to begin shipping the vaccine to the European Union in the first quarter of 2022. The WHO’s EUL—the ninth for a SARS-CoV-2 vaccine—is for a version of the vaccine manufactured and marketed by the Serum Institute of India (SII), under license from Novavax, known as Covovax. The WHO listing allows the COVAX facility to distribute the vaccine with hopes of bolstering global vaccine supply. Covovax—an adjuvanted, recombinant spike protein nanoparticle vaccine—is less expensive and simpler to manufacture than some of the other vaccine types and easier to distribute, as it can be stored for 6 months in normal refrigeration.
The New England Journal of Medicine last week published results from a phase 3 clinical trial testing the vaccine in nearly 30,000 adults in the US and Mexico, showing vaccine efficacy against symptomatic infection to be 90.4%, with 100% efficacy against moderate-to-severe disease. Most of the COVID-19 cases sequenced in the study were caused by B.1.1.7 (Alpha), and the vaccine’s efficacy against any variant of concern (VOC) or interest was 92.6%. The vaccine’s efficacy against the new Omicron VOC is unknown, but having another effective vaccine is important in helping to control the pandemic. In November, Indonesia was the first country to grant emergency use authorization (EUA) to the Novavax vaccine, followed by the Philippines. The company has plans to apply for an EUA with the US FDA by the end of the year.
PFIZER-BIONTECH VACCINE IN YOUNG CHILDREN Pfizer-BioNTech last week released an update on its ongoing phase 1/2/3 study evaluating their SARS-CoV-2 vaccine among children ages 6 months to under 5 years of age. An immunogenicity analysis showed that 1 month after the second 3 µg dose of the vaccine, participants aged 2 to under 5 did not show a robust immune response to the lower-dose shots when compared to the immune responses seen in older teens and young adults. The companies said the trial will continue but they plan to evaluate a third 3 µg dose of vaccine administered at least 2 months after the second dose to all age groups in the study, with the hope that a 3-dose regimen will elicit more protective immune responses. The companies said no safety concerns have arisen. The data have not been released publicly and many questions remain, including what the immune response was in the 2 to under-5 age group, if any.
The shift in plans also pushes back the companies’ expected timeline to submit results to the US FDA from the end of this year to the second quarter of 2022, if the results are positive. They also announced plans to test a third dose of the already authorized 10 µg formulation in children ages 5 to 12 years; a trial to evaluate a third dose of 10 µg or 30 µg in adolescents ages 12 to 17 in order to assess safety and immunogenicity; and the development of an Omicron variant-specific vaccine. The companies also last week filed with the FDA to request that adolescents ages 12 to 15 years be included in the vaccine’s full approval, with filings in the European Union and other regulatory authorities expected soon. The Pfizer-BioNTech vaccine, known as Comirnaty, received full FDA approval as a 2-dose (30 µg) regimen for individuals ages 16 years and older in August.
“TEST TO STAY” GUIDANCE The US CDC on December 17 said unvaccinated students exposed to a person with COVID-19 can remain in school if they are tested twice in the week following exposure and both tests are negative. The new guidance, known as “test to stay,” is an effort to keep children in school instead of having to quarantine at home and miss class, while also alleviating the burden on parents to arrange child care. The new protocol—which should be used as one method in a layered prevention approach—is based on 2 studies published in the CDC’s Morbidity and Mortality Weekly Report (MMWR), one examining the policy in Los Angeles County, California, and the other in Lake County, Illinois. The studies were conducted prior to the detection of the fast-spreading Omicron variant of concern, but CDC officials said they have confidence the mitigation strategy will work and will update guidance as needed. Agency officials also urged parents to vaccinate their children if they are eligible, as it remains the best way to prevent infection or severe disease. Under current CDC guidance, vaccinated people do not have to quarantine after a known exposure unless they have symptoms but should be tested 5-7 days after the exposure and wear a mask until testing negative.
US VACCINE MANDATES A federal appeals court last week lifted the stay on the Biden administration’s “vaccine or test” COVID-19 mandate for businesses with 100 or more employees, prompting confusion over whether companies need to comply with the Occupational Safety and Health Administration (OSHA) temporary rule. Following the order, several appeals were filed with the US Supreme Court requesting Justice Brett Kavanaugh, who has jurisdiction over the appeals court that lifted the stay, to consider the rule and immediately enjoin enforcement of the rule. Justice Kavanaugh likely will refer the case to the full court, and the justices have not acted on the emergency request. The Supreme Court asked the Biden administration to file its response by December 30, and the court is expected to make a decision in early 2022. Separately, the Biden administration has asked the court to stay lower-court decisions enjoining enforcement of a Centers for Medicare and Medicaid Services (CMS) vaccine mandate for healthcare workers. The Supreme Court has generally supported vaccine mandates implemented by state governments and universities but shown more nuance when considering federal pandemic-related rules.
Meanwhile, the US Armed Forces are beginning disciplinary actions, including dismissals, for members of the military who have not yet been vaccinated. As many as 20,000 troops risk being discharged. The US Department of Defense also is requiring members of the National Guard to be vaccinated against COVID-19. But governors from 5 states—Iowa, Wyoming, Alaska, Mississippi, and Nebraska—are pushing back on the mandate, arguing in a letter that National Guard members fall under the jurisdiction of their state, unless they are federally deployed, and would therefore not be subject to federal mandates. The Defense Department has not responded to the letter. Notably, the department last month rejected a request from Oklahoma Governor Kevin Stitt to exclude the state’s National Guard members from the federal mandate, instead releasing new guidance saying members who refuse vaccination will receive a general officer memorandum of reprimand, which could be grounds for administrative separation.
MODERNA VACCINE PATENT DISPUTE Moderna has paused a dispute with the US government by not taking the final step in obtaining a patent for technologies used in its SARS-CoV-2 mRNA vaccine. The company said making the payment to obtain the patent “could interfere with further discussions aimed at an amicable resolution” with the US National Institutes of Health (NIH) and wanted to “avoid any distractions” in ongoing collaboration amid efforts to respond to the quickly spreading Omicron variant of concern (VOC). At issue is who should be credited with developing the genetic sequence technology used in the company’s mRNA vaccine. Scientists from Moderna and NIH worked quickly in early 2020 to invent the technology, but Moderna has disputed claims that the NIH researchers are co-inventors. Moderna maintains that only its scientists deserve credit and has filed an application to pursue a patent at a later date. Moderna is projected to bring in as much as US$18 billion in sales of the vaccine this year and has been under increasing pressure to share its vaccine technology with low- and middle-income countries in order to increase global supply. At this time, it is unclear whether Moderna’s decision to pause its patent application has implications for the US government’s global vaccination strategy.