COVID-19
Updates on the emerging novel coronavirus pandemic from the Johns Hopkins Center for Health Security.
The Center for Health Security is analyzing and providing updates on the emerging novel coronavirus. If you would like to receive these updates, please subscribe below and select COVID-19. Additional resources are also available on our website.
EPI UPDATE The WHO COVID-19 Situation Report for July 23 reports 15.01 million cases (247,225 new) and 619,150 deaths (7,097 new). This is the second highest global daily total to date, and it is 21,044 more new cases than the same day the previous week (226,181 cases on July 16). Based on this trend, we expect the WHO to report record high global incidence today and/or tomorrow.
After recent data indicated that it was reaching a peak or plateau, Brazil reported its 2 highest daily totals over the past 2 days—67,860 and 59,961 new cases, respectively. These are considerably higher than the highest days in recent weeks, which were consistently around 45-46,000 new cases. Brazil remains #3 globally in terms of daily incidence, but it closed the gap with India. Colombia reported 7,945 new cases, its fourth highest daily incidence to date. Colombia is currently #5 globally with respect to daily incidence. Mexico reported 8,438 new cases, its highest daily incidence to date. Mexico is #6 globally in terms of daily incidence. Broadly, the Central and South American regions remain major COVID-19 hotspots. Including Brazil, Colombia, and Mexico, the region represents 5 of the top 10 countries globally in terms of daily incidence, along with Argentina (#8) and Peru (#9). Multiple other countries in the region are reporting more than 1,000 new cases per day. Additionally, the region includes 4 of the top 10 countries in terms of per capita daily incidence—Panama (#3), the US (#5), Brazil (#8), Colombia (#9)—and a number of other countries are reporting more than 100 new daily cases per million population.
India reported nearly 50,000 new cases, doubling its daily incidence since July 9. India remains #2 globally in terms of daily incidence. Bangladesh continues to report slowly decreasing daily incidence; however, it is also reporting decreased testing while its test positivity remains steady, slightly above 20%. This could indicate that Bangladesh's decreased incidence could be driven more by reduced testing than slowing transmission. Bangladesh remains #10 globally in terms of daily incidence.
South Africa reported 13,104 new cases, and it remains among the top countries globally in terms of both per capita (#4) and total daily incidence (#4).
The Eastern Mediterranean region remains a global COVID-19 hotspot, particularly with respect to per capita daily incidence. Oman is currently the only country averaging more than 250 new cases daily per million population*. The region represents 4 of the top 12 countries globally—Oman (#1), Bahrain (#2), Kuwait (#11), and Qatar (#12). Nearby Israel (#6) and Armenia (#10), both in the WHO’s European region, are among the top countries globally as well. While no countries in the region are in the top 10 in terms of total daily incidence, many are reporting more than 1,000 new cases per day.
*With the exception of Kyrgyzstan, which reported a single-day spike on July 18 before returning to its normal level.
Russia continues to report steadily declining daily incidence, but it remains #7 globally. Luxembourg is #7 globally in terms of per capita daily incidence.
UNITED STATES
The US CDC reported 3.95 million total cases (70,106 new) and 142,755 deaths (1,078 new). On July 22, the CDC reported more than 1,000 deaths for the first time since early June, and it has now exceeded that threshold for the second consecutive day. The US could potentially surpass 150,000 deaths by the end of next week. Additionally, both of the last 2 updates exceeded the daily incidence for the corresponding day from the previous week by more than 2,000 cases. The 7-day average daily incidence is 66,920 cases, the country’s highest to date, indicating that daily incidence continues to increase, even if it is potentially beginning to level off.
More than half of US states have reported more than 40,000 total cases, including California and New York with more than 400,000 cases; Florida and Texas with more than 350,000; and 8 additional states with more than 100,000. The US fell to #5 globally in terms of per capita daily incidence, but it remains #1 in terms of total daily incidence.
We expect the US to surpass 4 million cumulative cases in this afternoon’s update. From the first case reported in the US on January 22, it took 81 days to reach 500,000 cases and 98 total days to reach 1 million cases. From there:
1 million to 2 million cases: 44 days
2 million to 3 million cases: 27 days
3 million to 4 million cases: 14 days
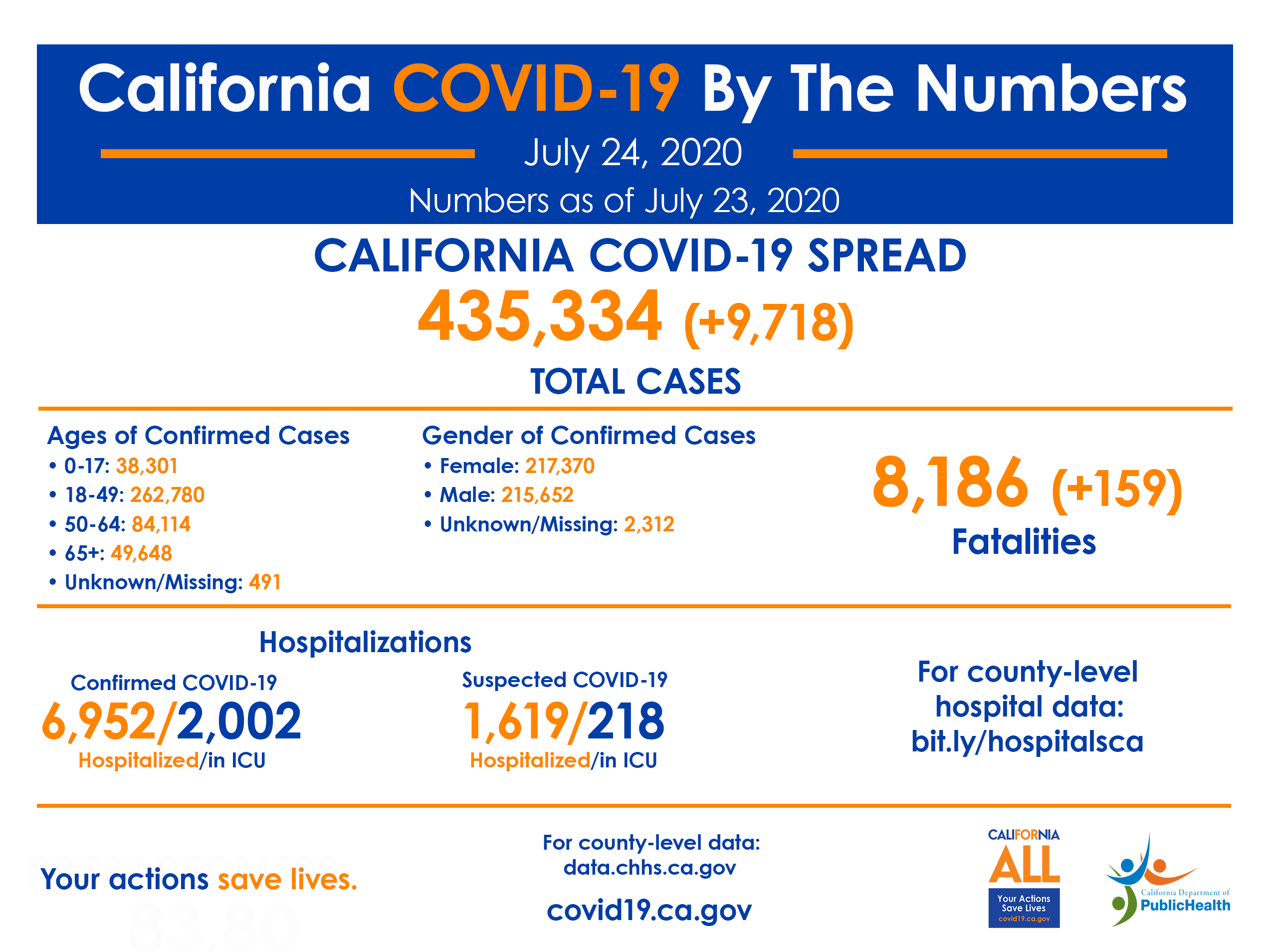
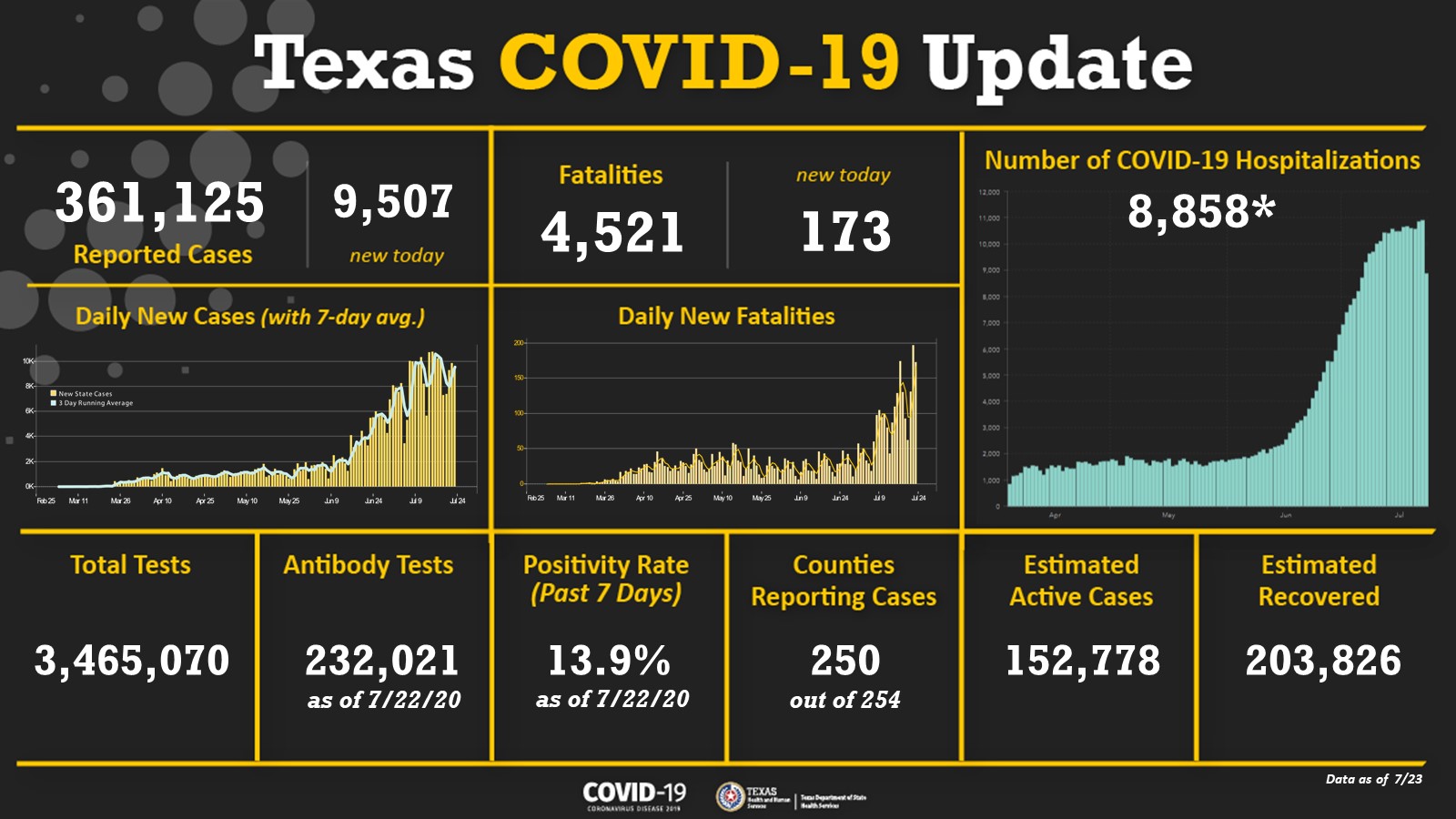
California (425,616 cases) surpassed New York (410,450 cases) to become #1 in the US in terms of cumulative COVID-19 incidence. With an average daily incidence of more than 11,000 cases, we expect Florida (402,312 cases) to surpass New York today, and with approximately 10,000 new cases per day, Texas (361,125 cases) could surpass New York by the middle-to-end of next week. California (nearly 10,000 new cases per day) could surpass 500,000 cumulative cases by the end of next week.
The Johns Hopkins CSSE dashboard reported 4.06 million US cases and 144,552 deaths as of 12:30 pm on July 24.
NIH CLINICAL TRIALS The US NIH is initiating several clinical trials as part of the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) public-private partnership. Initiated on April 17, the goal of this effort is to develop a coordinated research strategy to speed up the development of COVID-19 candidate pharmaceuticals. ACTIV has 4 fast-track areas of focus, including pre-clinical treatments, accelerating clinical testing for vaccines and treatments, improving clinical trial capacity, and accelerating evaluation of vaccine candidates. The new trials include antiviral monoclonal antibodies, for both hospitalized and at-home patients; drugs to reduce dangerous inflammatory responses to COVID-19; and drugs to treat blood clotting. A principal goal of the program is to ensure coordinated and standardized protocols and study designs across multiple testing sites in order to promote robust analyses. More than 1,200 clinical trials have been registered with the US government for COVID-19 drugs, and nearly 40% of them involved fewer than 100 patients. This disorganized approach likely will not yield robust data to support effective analysis of many candidate drugs, and ACTIV aims to improve consistency and coordination nationwide.
NIH Director Dr. Francis Collins and several NIH colleagues published a special report in The New England Journal of Medicine that outlined the Rapid Acceleration of Diagnostics program (RADx), led by NIH in partnership with other US government entities, including the Biomedical Advanced Research and Development Authority (BARDA) and the Department of Defense. RADx was conceived to support rapid development and production of novel diagnostics, including the use of “innovative diagnostic technologies.” Perhaps most notably, it is “expressly focused on health disparities,” rather than purely technical challenges. The program includes 4 principal components, each with a specific focus. Three of the components focus on technical aspects of product research, development, and production, and the fourth is dedicated to improving equity among underserved populations. Racial and ethnic minorities are disproportionately affected by COVID-19, and this component, RADx-UP, aims to characterize the factors driving this elevated burden and improve access to testing among high-risk populations, including through community engagement activities.
US COVID-19 RESURGENCE The US continues to battle a resurgence of COVID-19, driven largely by states that were not severely affected early in the US epidemic. As noted above, the US reported 1 million cases over the past 2 weeks alone, and numerous states are exhibiting concerning trends. Current data indicate stark regional differences in the severity of the current COVID-19 resurgence. States in the Northeast, including New England and the Mid-Atlantic region—particularly the northern portion, including Connecticut, New Jersey, and New York—appear to be faring considerably better than the South, Southwest, West, and Midwest. These differences are evident across all major indicators, including incidence, mortality, test positivity, and hospitalizations.
Increasing COVID-19 hospitalizations, in particular, have garnered considerable attention, following reports that hospitals and health systems are struggling to meet the COVID-19 patient surge. Newly published data from HHS shows multiple states in these severely affected regions reporting more than 25% of inpatient hospital beds currently occupied by COVID-19 patients, including Arizona, California, Georgia, New Mexico, and Texas. Several other states in the South, Southwest, and West—including Alabama, Arkansas, Louisiana, Mississippi, Nevada, and South Carolina—are reporting that more than 15% of inpatient beds are occupied by COVID-19 patients. Additionally, analysis from the COVID Tracking Project indicates that national COVID-19 hospitalizations are now equal to the country’s first peak in mid-April. In the first peak, COVID-19 cases were largely concentrated in a few major metropolitan areas—including Boston, Detroit, and New York—and overwhelmed local health systems, which accounts, to some degree, for the higher per capita incidence in these areas. Now, the cases are spread out across a much larger geographic area and population, and more hospitals and health systems, and the overall mortality is lower than it was early in the US epidemic (although beginning to increase again). If continued uncontrolled transmission continues, however, it could necessitate spreading limited health resources (eg, mechanical ventilators, investigational treatment drugs) more thinly across the country, which could exacerbate recent increases in mortality. Statistically speaking, some portion of hospitalized patients are expected to die from COVID-19, so as hospitalizations increase, so will COVID-19 mortality, particularly if available resources are exhausted.
These state- and regional-level disparities have driven a number of states to implement domestic travel advisories or restrictions. Some states require arriving travelers to be tested for SARS-CoV-2 and/or provide documentation of a recent negative test, and some require or recommend self-quarantine, typically for 14 days. Some of these requirements pertain to specific states, and others are broadly applied to all out-of-state travelers. Connecticut, New Jersey, and New York previously implemented a joint policy that requires travelers arriving from severely affected states to quarantine themselves for 14 days upon arrival. The initial list was relatively limited, with only 9 affected states; however, it has ballooned to more than 30 states, covering approximately two-thirds of the entire US population. Additionally, the Ohio Department of Health issued a similar travel advisory for any state reporting test positivity of 15% or greater. The new Ohio policy currently covers 9 states. The Ohio Department of Health recommends 14-day self-quarantine and temperature/symptom monitoring for individuals with recent travel to the affected states, but it does not appear to be mandatory. Interestingly, it appears that Florida’s mandatory quarantine for travelers arriving from the New York tri-state area, implemented earlier in the US epidemic, remains in effect, despite the fact that Florida is currently reporting more than 11 times the combined daily incidence of New York, New Jersey, and Connecticut.
In response to surging COVID-19 incidence in Florida, US President Donald Trump announced that activities for the Republican National Convention scheduled in Jacksonville will be cancelled. Some convention activities were originally moved from Charlotte, North Carolina, after disagreements regarding the state’s restrictions on large gatherings; however, Republican delegates will reportedly still meet in Charlotte to announce President Trump as the Republican nominee for the 2020 presidential election.
INTERNATIONAL COVID-19 RESURGENCE In addition to the US, some other countries are beginning to experience their own COVID-19 resurgence. Many countries are still experiencing the effects of their initial wave of transmission; however, some countries that previously contained their epidemic are now facing increased transmission, some on a national scale and others more localized. Both Tokyo, Japan, and Melbourne, Australia, are reporting major outbreaks, which have resulted in the need to re-institute some social distancing restrictions—although not to the level of full “lockdown.” Spain, one of the most severely affected countries early in the pandemic is now exhibiting increased transmission again, following the relaxation of nationwide social distancing policies. These increases are much smaller than those observed in the US, but they are concerning nonetheless. In the absence of a vaccine, any increase in social contact will result in increased transmission, so it is likely that we will continue to observe this trend as national, regional, and local governments attempt to strike the right balance between COVID-19 risk and economic and social benefits.
Despite early success in containing its COVID-19 epidemic, South Africa has also recently exhibited a resurgence of COVID-19. Notably, South Africa is reporting an increase in excess all-cause mortality, which could potentially be the result of redirecting healthcare resources and services toward the COVID-19 response. While the country’s COVID-19 deaths now exceed 6,000, excess deaths related to natural causes have surpassed 17,000. South Africa accounts for more than half of all COVID-19 cases on the African continent. With the surge in COVID-19 incidence, South African President Cyril Ramaphosa decided to close schools for several weeks. President Ramaphosa also implemented a temporary ban on alcohol sales and a mandatory curfew in the hopes that a decrease in alcohol-related incidents will make more hospital beds available for COVID-19 patients and others. Many hospitals in highly populated areas are already reaching their capacity, and oxygen supplies running low.
US ECONOMIC STIMULUS The US government continues to evaluate options for a possible “Phase 5” COVID-19 funding bill, but considerable uncertainty remains regarding the content and timeline. Senate Majority Leader Mitch McConnell was expected to release a draft bill this week as a starting point for debate in the Senate, but it appears that it may be delayed until at least next week as details are finalized. The funding bill could potentially provide support for hospitals and health systems and state and local governments as well as individuals. Individual stimulus payments and expanded federal unemployment benefits are among a long list of high-profile priorities. A report by The Hill indicates that the Senate bill is expected to include similar stimulus payments as the previous phase of funding, possibly US$1,200 per person for everyone with an annual income of $75,000 or less. Senator McConnell previously suggested that the income cap could be lowered for this round to US$40,000, but there are indications that this may have changed.
Considering that the current expanded federal unemployment insurance, an extra US$600 per week, is scheduled to expire next week, it is possible that individuals receiving those benefits could lose that additional funding for a period of weeks while a bill is finalized and implemented. It is unclear if any temporary measures are being evaluated to prevent these payments from lapsing. The Senate bill will reportedly not include a payroll tax cut for businesses, previously a priority for President Trump, following opposition from Republican Senators. Again, these negotiations are ongoing, and the Senate draft has yet to be finalized and released. The House of Representatives passed its own funding bill several weeks ago, but there will likely be substantial differences between the House and Senate proposals. There appears to be pressure to reach an agreement soon in order to provide economic support as states continue to maintain, and in some cases strengthen, social distancing policies, but the exact path forward is not clear at this time.
SAFER NEUTRALIZATION ASSAY There are many different kinds of SARS-CoV-2 serological tests, all of which detect the presence of immune response to previous SARS-CoV-2 infection. Neutralization assays detect neutralizing antibodies, or antibodies that correspond to protective immunity. Because neutralization assays require live virus in order to challenge the patient’s antibodies in culture, most of these tests must be performed in high-containment laboratory settings. High-containment laboratories are less common than those operating under lower biosafety levels, so critical research on protective immunity via neutralizing antibodies has been slow.
A study published in Nature presents a surrogate viral neutralization test (sVNT) that can be performed at the BSL-2 level, as opposed to the BSL-3 level. In the sVNT protocol, conjugated SARS-CoV-2 receptor binding domain and patient blood serum are added to an ELISA plate coated in human ACE-2 receptor. If the patient serum contains neutralizing antibodies, they will block the binding action of the receptor binding domain to the human ACE-2 receptor, which can be quantified using indirect ELISA techniques. The researchers demonstrated that the sVNT protocol exhibited high correlation with results obtained from conventional VNT and pseudovirus VNT techniques. This assay and others like it could accelerate research on protective immunity as the pandemic progresses by allowing it to be conducted in more laboratories and at lower biosafety levels.
US CDC SCHOOL GUIDANCE As the US moves toward the scheduled start of the 2020-21 school year, the US CDC published several updated guidance documents to support schools in preparing for classes in the midst of the COVID-19 pandemic. A number of prominent US government officials, including President Trump, have publicly called for schools to resume in-person classes, but many state governments, school officials and teachers, and health experts warn that might not be feasible or safe in some circumstances. The updated guidance includes information for schools regarding the current understanding of COVID-19 risk to children and their role in driving transmission in the community and at home as well as recommendations for implementing appropriate social and physical distancing (including mask use), enhanced hygiene and sanitation, and disease surveillance and monitoring systems. The guidance also includes considerations based on the current level of community transmission, including the possible need to close schools due to uncontrolled community spread. In addition to schools, the CDC offers tools and information aimed at parents to help evaluate risk.
The updated CDC guidance includes a statement that explicitly emphasizes the importance of in-person school for children. Some media reports have characterized this as a push by the CDC to resume in-person classes during the pandemic, as it focuses primarily on the benefits of in-person learning rather than public health considerations related to COVID-19. The statement highlights the disproportionate impact of remote classes on lower-income students, racial and ethnic minorities, and students with disabilities or special needs as well as the importance of services schools provide beyond education that support these and other students. Notably, the CDC emphasizes repeatedly that the risk to students—including direct health risks to children and risks of spreading the disease at home—are relatively low in communities with low levels of SARS-CoV-2 transmission. The statement largely focuses on the impact for students and does not fully address the risks to teachers, staff, and family members.
COVID-19 IN REFUGEE POPULATIONS As the COVID-19 pandemic continues, it is clear that some populations are at elevated risk of infection, severe disease, and death, in particular, racial and ethnic minorities. Refugee populations face even greater risk, stemming from conditions in densely populated refugee camps, barriers to accessing health services (including investigational treatment drugs), pre-existing health conditions and poor nutrition, other communicable disease risks (eg, cholera), and limited access to reliable infrastructure like clean water. Additionally, the pandemic is limiting international aid for these populations, as donor countries focus resources domestically to control their own epidemics. Reduced humanitarian aid, including for routine immunizations, can compound the health impact of COVID-19, especially for children, who suffer most during humanitarian crises. Experts at Johns Hopkins University will host a webinar on July 29 (1pm EDT/5pm GMT) to discuss the impact that COVID-19 is having on refugee populations and the response efforts needed to protect children, including through routine immunizations and a potential COVID-19 vaccine. The speakers will include Dr. Shaun Truelove from the Johns Hopkins International Vaccine Access Center and Dr. Paul Spiegel, Director of the Johns Hopkins Center for Humanitarian Health. Advance registration is required to participate.