This is a work in Progress

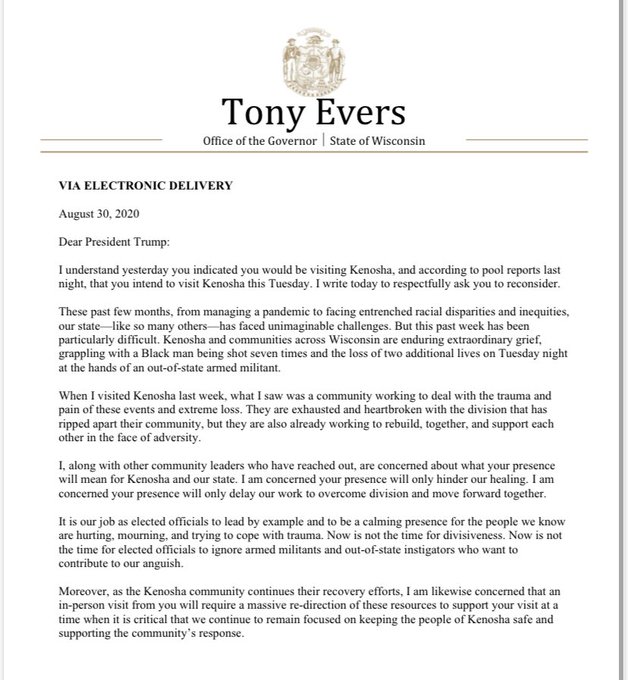
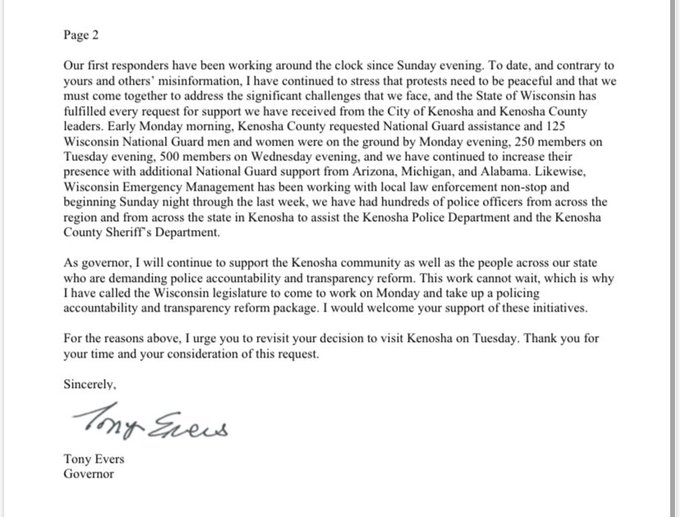
The projections from August 6 and August 21,are projects through December 1, 2020.* The other four projections are through November 1, 2020, Georgia has the highest projected death rate 2708 per million. Projections rose by major proportions for Massachusetts, Arizona, District of Columbia, California, Illinois, South Carolina, Pennsylvania, Iowa, and North Dakota. Decreases for Missouri, Kansas, Virginia and Wisconsin.
The August 21 projections are available from: https://covid19.healthdata.org/united-states-of-america
July 7----July 14-----JULY 22------July 30—August 6*—August 21*—August 27*
United States 208,255, 224,546, 219,864, 230,822, 295,011, 309,918; NOW 317,312 Population 331.00 million 629.17 per million 678.39 per million, 664.24 per million, 697.35 per million, 891.17 per million, 936.3 per million, NOW 958.65 per million
Georgia 3,857 deaths; 4736; 7336; 10,278, 11,288, 10.805, NOW 12,410 Population 3.99 million 966.67 per million ; 1186 .97 per million;1838.60 per million; 2575.94 per million; 2829.07 per million; 2708.02 per million; NOW 2110.28 per million
Massachusetts 12,906 deaths; 10,121 deaths ; 9970; 9647; 10,314; 12.295, NOW 12,410 Population 6.7 million 1926.27 per million 1510.60 per million; 1488.06 per million; 1439.85 per million; 1539.40 per million; 1835.07 per million; NOW 1852.24 per million
New York 32,221 deaths; 35,379; 35,039; 34,423; 33,945; 32,743, NOW 33,960 Population 18.8 million 1713.88 per million; 1881.86 per million; 1863.78 per million; 1836.33 per million; 1805.59 per million; 1741.65 per million; NOW 1806.38 per million
Louisiana 4,643 deaths; 5,167; 4955; 6401; 7901; 7840; NOW 7993 Population 4.6 million 1009.35 per million; 1123.26 per million; 1077.17 per million; 1391.52 per million;1717.61 per million; 1704.35 per million; NOW 1737.61 per million
California 16,827 deaths; 21,264; 19,572; 16,515; 32,692; 41,110; NOW 37,645 Population 39.78 million 423.00 per million; 534.54 per million;492.01 per million; 415.16 per million; 821.82 per million; 1033.43 per million; NOW 1497.52 per million
District of Columbia 666 deaths; 681 ; 694 ; 646; 605; 837; NOW 935 Population .706 million 943.34 per million; 964.59 per million; 983.00 per million; 915.01 per million; 856.94 per million; 1185.55 per million; NOW 1324.36 per million
Connecticut 4,692 deaths; 4,456; 4750; 4844; 5179; 4675; NOW 4626 deaths Population 3.7 million 1268.11 per million; 1204.32 per million;1283.78 per million; 1309.19 per million; 1399.73 per million; 1263.52 per million; NOW 1250.27 per million
Illinois 8,907 deaths; 8,351; 8472 ; 8280; 9995; 11,071, NOW 15,058 Population 12.63 million 705.23 per million; 657.56 per million; 772.43 per million; 655.58 per million; 791.37 per million; 876.56 per million, NOW 1192.24 per million
Pennsylvania 9,999 deaths; 8,431; 8028; 8350; 8859; 14,998; 14,604; NOW 14,604 Population 12.7 million 787.32 per million; 663.86 per million; 632.13 per million;657.48 per million; 697.56 per million; NOW 1180.94 per million;
Florida 17,477 deaths;19,285; 18,154, 16,318; 19,358; 21,174; NOW 24,532 Population 21.47 million 814.01 per million; 893.23 per million; 845.55 per million; 760.04 per million; 901.63 per million; 986.21 per million; NOW 1142.63 per million
South Carolina 242 deaths; 4,556; 3186; 3232; 3672; 4724; NOW 5023 Population 5.0 million 48.4 per million; 911.20 per million; 637.2 per million;646.4 per million; 734.40 per million; 944.8 per million; NOW 1004.60 per million
Arizona 5,553 deaths; 5,177; 5664;7946; 6840; 9562; NOW 7148; Population 7.29 million 761.73 per million ;710.15 per million; 776.95 per million: 1089.97 per million; 938.27 per million.; 1311.66 per million; NOW 980.52 per million;
Iowa 841 deaths; 1,225; 1813,1700; 2163 2856; NOW 3077 Population 3.17 million 265.30 per million; 386.44 per million; 571.93 per million; 536.28 per million; 682.34 per million; 900.95 per million; NOW 970.66 per million
Texas 13,450 deaths;18,675; 18,812; 24,557; 27,435; 25.532; NOW 27,194 Population 29.90 million 449.83 per million; 624.58 per million; 629.16 per million; 921.30 per million; 917.56 per million; 853.91 per million; NOW 909.50 per million
Missouri 5436 deaths; 3068; NOW 5231 Population 6.137 million; 885.77 per million; 499.92 per million, NOW 852.37 per million
Arkansas 724 deaths; 617, 895; 833; 2234; 2364; NOW 2406 Population 3.018 million 239.89 per million 204.44 per million; 293.55 per million; 276.01 per million ; 740.23 per million; 783.30 per million; NOW 797.22 per million
Oklahoma 587 deaths;1,029 ; 1533; 1484; 2967, 2058; NOW 3055 Population 4.0 million 146.75 per million 257.23 per million; 383.25 per million; 371.24 per million; 741.75 per million; 514.5 per million; NOW 763.75 per million
Maryland 3,880 deaths ; 4,278; 4194; 4026; 5174; 5301; NOW 4404 Population 6.0 million 646.67 per million; 713.00 per million; 699.0 per million; 671.0 per million; 862.34 per million; 883.5 per million; NOW 734 per million
Ohio 5,712 deaths;4,545; 3900; 5694; 9041; 6046; NOW 7564 Population 11.73 million 486.96 per million; 387.47 per million; 332.48 per million; 485.42 per million; 770.76 per million; 515.43 per million; NOW 644.84 per million
North Dakota 215 deaths; 371; NOW 491 Population .762 million 282.15 per million;486.88 per million; NOW 644.36 per million
Washington 2,510 deaths; 3,170; 3303; 2178; 5078; 5040; NOW 4410 Population 7.17 million 325.98 per million ;442.112 per million; 450.67 per million; 303.77 per million; 708.23 per million; 702.93 per million; NOW 615.06 per million
Oregon 471 deaths; 605; 683; 634; 2967; 2408; NOW 2395 Population 4.3 million 109.53 per million 140.70 per million; 158.84 per million; 147.44 per million; 690.0 per million; 560.0 per million; NOW 556.98 per million
Colorado 1937 deaths; 2,032; 2774: 2665; 5179; 2967; NOW 2395 Population 5.8 million 333.97 per million; 478.28 per million; NOW 459.48 per million; 892.93 per million’ 511.55 per million; NOW 412.93 per million
Wisconsin 1,410 deaths; 992; 1041; 2030; 3708 ;1775; NOW 2340 Population 5.82 million 242,27 per million 170.45 per million; 178.87 per million; 348.80 per million; 637.11 per million ; 304.98 per million; NOW 402.06 per million
Kansas 632 deaths ; 410; 412; 588; 2245; 1277; NOW 994 Population 2.77 million 228.16 per million 148.01 per million; 148.74 per million; 212.27 per million; 810.47 per million; 461.01 per million; NOW 358.84 per million
Virginia 5,190 deaths ; 4,881; 2643; 2289; 5842; 2828; NOW 2940 Population 8.63 million 601.39 per million ;565.59 per million; 306.26 per million: 265.24 per million; 676.94 per million; 327.69 per million; NOW 340.67 per million
South Dakota 254 deaths; 281; NOW 291 Population .885 million 287.01 per million;317.51 per million; NOW 328.81 per million
Idaho 120 deaths; 559; 513; 365; 916, 983: NOW 1373 Population 4.3 million 109.53 per million 140.70 per million; 158.84 per million;147.44 per million; 213.02 per million; 228.60 per million; NOW 319.30 per million
DEATHS
How many overall deaths will there be?
Our model is updated to account for new data and information, and the estimates may change as a result. For the latest estimate, visit our COVID-19 projections tool.
Why do your results show a wide range in the forecast for deaths?
Larger uncertainty intervals – or the range within which estimated deaths are likely to fall – can occur because of limited data availability, small studies, and conflicting data. A smaller range generally reflects extensive data availability, large studies, and data that are consistent across sources.
Why did the estimates for my location change?
To learn more, please visit our update page.
Why is the peak for daily deaths still forecast in the future when it looks like it has already occurred in my location?
The date of peak daily deaths depends on the model’s projections. If the model projects that the number of daily deaths will continue to rise, then the peak will be projected for a future date. It is important to note that the data on daily deaths may fluctuate dramatically due to irregularities in reporting. Health care workers are extremely busy caring for COVID-19 patients, so they may fall behind on reporting deaths. Once health care workers catch up on their reporting, however, it may appear as though there has been a spike in daily deaths.
Why are the “observed deaths” shown in your results for my location different from what is shown on the government’s official page?
For deaths, we primarily use the COVID-19 death data aggregated by the Johns Hopkins University (JHU) data repository (see "Where does IHME obtain its data?"). The JHU repository uses Coordinated Universal Time (UTC), which means new days start at 8 p.m. Eastern time. The JHU counts may differ slightly from local government data as a result of these timing differences. Also, the JHU repository is not necessarily synchronized to the update schedule of every location, so there may be a short lag that is reflected in a difference between our recorded daily deaths in a given location and those ultimately reported on government websites. Although this will be corrected when we update our analysis, in some cases, these differences may persist for several days.
Yet another reason why observed deaths may differ from numbers reported by governments is due to data processing. To address irregularities in the daily death data, we average data from the last three days to create a smooth version. To see the death data exactly as it is reported, 1) click the “Chart settings” icon in the upper right corner of the chart, and 2) turn off “Smoothed data.”
There are reports of deaths being under-reported in places. How does this impact your forecast?
We are learning that not all deaths due to COVID-19 that occur at home or in nursing homes have been attributed to COVID-19. As awareness increases, the number of reported deaths is growing, with some locations now reporting presumptive COVID-19 deaths. Another challenge is that COVID-19 death data fluctuate substantially each day, with some locations reporting more deaths on Tuesdays than on Sundays and Mondays. We believe this variation is due to data reporting practices instead of actual death patterns. To mitigate the impact of inconsistent reporting on our forecasts, our published predictions are based on averaging multiple iterations of projections. As new data emerges, we incorporate it into our model, and our projections will shift up or down in response to the data. To learn more, see our estimation updates.
For Ecuador and Peru in particular, the number of reported deaths due to COVID-19 appears to be improbably low. Instead of using reported COVID-19 deaths for these countries, we are approximating deaths from COVID-19. To approximate COVID-19 deaths, we used the number of excess deaths occurring in Ecuador and Peru during the COVID-19 pandemic and observations from other countries where we had weekly reports of total deaths and high-quality data on COVID-19 deaths.