Narcissistic Personality Disorder DSM-5 301.81 (F60.81)
DSM-5 Category: Personality Disorders
Introduction
Narcissistic personality disorder (NPD), a cluster B personality disorder, is considered to be one of the least identified personality disorders (Pies, 2011). On the other hand, a good number of patients with narcissistic traits present at the psychiatrist's office with other types of issues such as anxiety or depression. A common finding in clinical practice, NPD frequently coexists with other psychiatric disorders. NPD is a relatively recent diagnostic category. Its origins stem from a great effort between psychoanalysts and psychoanalytic psychotherapists to recognize a cluster of predominantly difficult patients who could not be classified as psychotic, not typically neurotic and overall not responsive to conventional psycho therapeutic treatment options (Gildersleeve, 2012).
NPD appears to be more widespread in males than females for unknown reasons. In the past there has been some speculation that the limited spotlight on grandiosity likely adds to the extensive discrepancy that is seen with small NPD prevalence rates in epidemiological research and elevated occurrences of NPD seen in clinical practice (Campbell, Miller, & Widiger, 2010).
The most important characteristics of NPD are grandiosity, seeking excessive admiration, and a lack of empathy (Ronningstam & Weinberg, 2013). These identifying features can result in a negative impact on an individual’s interpersonal affairs and life general. In most cases, on the exterior, these patients act with an air of right and control, dismissing others, and frequently showcasing condescending or denigrating attitudes. Nevertheless, internally, these patients battle with strong feelings of low self esteem issues and inadequacy. Even though the typical NPD patient may achieve great achievements, ultimately their functioning in society can be affected as these characteristics interfere with both personal and professional relationships. A large part of this is as result of the NPD patient being incapable of receiving disapproval or rebuff of any kind, in addition to the fact that the NPD patient typically exhibits lack of empathy and overall disrespect for others.
Symptoms of Narcissistic Personality Disorder
The definition of NPD states that it comprises of a persistent manner of grandiosity, a continuous desire for admiration, along with a lack of empathy. It starts by early adulthood and occurs in a range of situations, as signified by the existence of any 5 of the next 9 standards (American Psychiatric Association, 2013):
- A grandiose logic of self-importance
- A fixation with fantasies of infinite success, control, brilliance, beauty, or idyllic love
- A credence that he or she is extraordinary and exceptional and can only be understood by, or should connect with, other extraordinary or important people or institutions
- A desire for unwarranted admiration
- A sense of entitlement
- Interpersonally oppressive behavior
- No form of empathy
- Resentment of others or a conviction that others are resentful of him or her
- A display of egotistical and conceited behaviors or attitudes
Another model, characterizes NPD as having fair or superior impairment in personality functioning, apparent by characteristic troubles in at least 2 of the following 4 areas (American Psychiatric Association, 2013):
- Individuality
- Self-direction
- Empathy
- Closeness
No actual physical characteristics are seen with NPD, but patients may have concurrent substance abuse, which may be seen in the clinical examination.
Epidemiology
Narcissistic Personality Disorder is more prevalent in males, with about 18 percent of males presenting with NPD, compared to six percent of females (Ronningstam & Weinberg, 2013). Within the general population, the prevalence rate is less than one percent, yet within the clinical population, this number rises to about 2 to 16 percent.
Differential Diagnosis
NPD has similar characteristics with the other 3 cluster B personality disorders, and thus should be differentiated accordingly. These are Antisocial personality disorder (ASPD), Borderline personality disorder (BPD) and Histrionic personality disorder (HPD). Additionally individuals with NPD may also meet the definition for also having axis I disorder, or exhibits features that similar to axis I disorders (CITE).
While no particular laboratory tests help with the diagnosis of NPD, a urine toxicology screen may be important to exclude substance abuse such as alcohol and drugs as likely reasons of the pathology.
Co-morbidity
Several comorbid disorders occur with NPD, with the most common being major depressive disorder, seen in about 45 to 50 percent of NPD patients (Ronningstam & Weinberg, 2013). Bipolar disorder presents in 5 to 11 percent of NPD patients (Ronningstam & Weinberg, 2013). On the other hand, the most prevalent comorbidity seen is that of substance abuse. Approximately 24 to 64.2 percent of NPD patients have substance abuse disorders (Ronningstam & Weinberg, 2013).
Treatment for Narcissistic Personality Disorder
The treatments for NPD are forms of therapy, as well as pharmacologic (Narcissistic Personality Disorder, 2011). The core of treatment lies with individual psychotherapy, which consists mainly of psychoanalytic psychotherapy. In addition, other types of therapy may be utilized, such as family, group, couples therapies, plus cognitive-behavioral therapy (CBT). Since NPD patients commonly have other psychiatric ailments like depression, anxiety or other mood disorders, certain psychotropic medications may also be administered.
While treatment for NPD largely remains outpatient, an indication for inpatient stay should occur if the patient severely worsens or becomes a threat to their own safety as well as others. Even with inpatient care, it is best to opt for shorter hospital times, as extended stays have not been reported to transform the course of the illness. The use of hospitalization ought to only be used as a short-term method which facilitates either the stabilization of environmental stressors, and/or regulation of drug dosages .
Psychotherapy
With individual psychoanalytic psychotherapy, much debate exists between the 2 key school of thoughts Kernberg and Kohut, both offering conflicting methods regarding the therapist’s role in treating NPD patients. Kernberg advocates a direct confrontation of the NPD patient during therapy, with the goal of eliminating or weakening the patient’s grandiosity. On the other hand, Kohut supports a more empathic role, that encourages the patient’s grandiosity, thus strengthening the patient’s naturally deficient self image (Gildersleeve, 2012). In therapy, a common form of treatment is a combination of both.
Other Forms of Therapy
Some speculate that NPD patients may experience difficulty handing group sessions, since they lack the traits needed for group therapy like patience, connectivity, and empathy. Research maintains that the use of long-term group therapy offers NPD patients the avenue to improve trust with others and other crucial relationship aspects in a safe and controlled environment (Ronningstam & Weinberg, 2013).
The use of Cognitive Behavioral Therapy (CBT) in treating NPD mainly involves the particular form of CBT recognized as schema-focused therapy, that focuses on fixing narcissistic schemas and the flawed moods and coping mechanisms (Matusiewicz, Hopwood, Banducci, & Lejuez, 2011).
Pharmacologic Therapy
No actual medications are indicated for the treatment of NPD. Given that patients may have other co-morbid psychiatric issues, these patients sometimes benefit from using medications such as antidepressants, antipsychotics, as well as mood stabilizers (Ronningstam & Weinberg, 2013).
Long-Term Monitoring
It is important for NPD patients to receive close long-term monitoring as there may be a potential risk for suicide, especially in patients who also have depression. While one can assume that giving the low self-esteem and high impulsive nature, suicidal behaviors should be directly linked with NPD (Campbell, Miller, & Widiger, 2010).
Social Impact
Ironically patients with NPD, also known as narcissists are reportedly happier than others in society. Being highly materialistic, self-enhancing, entitled and impulsive, they may not learn from mistakes, and have a tendency to get into even greater trouble, notably legal and disciplinary (Ronningstam & Weinberg, 2013). These maladaptive coping mechanisms can result in issues in the work place or in school, or unemployment.
Patients with NPD tend to be drawn to people of a high societal class, who think very highly of them (Campbell, Miller, & Widiger, 2010). The constant desire for admiration may cause romantic relationships to be short lived, as they constantly seek for something better, or when their lack of empathy becomes apparent to their partners (Ronningstam & Weinberg, 2013). So patients with NPD may exhibit an unforgiving nature and showcase anger and aggression in such close relationships (Ronningstam & Weinberg, 2013). This can also affect work relationships or any close group activities.
References
American Psychiatric Association. (2013). Personality disorders. In Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition ed.). Washington, DC: American Psychiatric Publishing Inc.
Campbell, W. K., Miller, J., & Widiger, T. (2010). Narcissistic Personality Disorder and the DSM–V. Journal of Abnormal Psychology, 119(4), 640 – 649. Retrieved March 7, 2014, from http://wkeithcampbell.com/wp-content/uploads/2013/08/MillerWidigerCampbell20101.pdf
Gildersleeve, M. (2012). Demystifying Paradoxical Characteristics of Narcissistic Personality Disorder. Indian Journal of Psychological Medicine, 34(4), 403-404. Retrieved March 7, 2014, from http://www.ijpm.info/article.asp?issn=0253-7176;year=2012;volume=34;issue=4;spage=403;epage=404;aulast=Gildersleeve
Matusiewicz, A., Hopwood, C., Banducci, A., & Lejuez, C. (2011, Sep 1). The Effectiveness of Cognitive Behavioral Therapy for Personality Disorders. Psychiatr Clin North Am, 33(3), 657–685. Retrieved March 7, 2014, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3138327/
Narcissistic Personality Disorder. (2011, Aug 29). Narcissistic Personality Disorder. Retrieved March 7, 2014, from Cleveland Clinic: http://my.clevelandclinic.org/neurological_institute/center-for-behavorial-health/disease-conditions/hic-narcissistic-personality-disorder.aspx
Pies, R. (2011, Feb). How To Eliminate Narcissism Overnight. Innovations in Clinical Neuroscience, 8(2), 23–27. Retrieved March 7, 2014, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3071092/
Ronningstam, E., & Weinberg, I. (2013, Spring). Narcissistic Personality Disorder: Progress in Recognition and Treatment. The Journal of Lifelong Learning in Psychiatry, XI(2), 167-177. Retrieved March 7, 2014, from http://focus.psychiatryonline.org/data/Journals/FOCUS/926935/167.pdf
Above is from: https://www.theravive.com/therapedia/narcissistic-personality-dis
SM-5 Category: Personality Disorders
Introduction
APD (Antisocial Personality Disorder) is a DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, fifth edition), diagnosis assigned to individuals who habitually and pervasively disregard or violate the rights and considerations of others without remorse. People with Antisocial Personality Disorder may be habitual criminals, or engage in behavior which would be grounds for criminal arrest and prosecution, or they may engage in behaviors which skirt the edges of the law, or manipulate and hurt others in non-criminal ways which are widely regarded as unethical, immoral, irresponsible, or in violation of social norms and expectations. Those with APD often possess an impaired moral conscience and make decisions driven purely by their own desires without considering the needs or negative effects of their actions on others. Impulsive and criminal behavior is common. The terms psychopathy or sociopathy are also used, in some contexts synonymously, in others, sociopath is differentiated from a psychopath, in that a sociopathy is rooted in environmental causes, while psychopathy is genetically based.
The term antisocial may be confusing to the lay public, as the more common definition outside of clinical usage is an individual who is a loner or socially isolated. The literal meaning of the word antisocial can be more descriptive to both the lay public and professionals. To be anti-social is to be against society: against rules, norms, laws and acceptable behavior. Individuals with Antisocial Personality Disorder tend to be charismatic, attractive, and very good at obtaining sympathy from others; for example, describing themselves as the victim of injustice. Some studies suggest that the average intelligence of antisocials is higher than the norm. Antisocials possess a superficial charm, they can be thoughtful and cunning, and have an intuitive ability to rapidly observe and analyze others, determine their needs and preferences, and present it in a manner to facilitate manipulation and exploitation. They are able to harm and use other people in this manner, without remorse, guilt, shame or regret. It is widely stated that antisocials are without empathy, however this can be disputed, as sadistic antisocials will use empathy to experience their victim's suffering, and derive a fuller pleasure from it (Turvey, 1995). This is depicted in the classic work A Cask of Amontillado by Poe, as the main character entombs another man alive “...then I heard the furious vibrations of the chain. The noise lasted for several minutes, during which, that I might hearken to it with the more satisfaction, I ceased my labours and sat down upon the bones.” (Poe, 1846 ). Some research also suggests that sociopaths and psychopaths do have degrees of empathy, but with an innate ability to switch it off at will. (Meffer, Gazzola, den Boer, Bartells, 2013). This connection to empathy may give hope to future successful treatment as it suggests individuals with APD may be trained.
Symptoms & Criteria for Antisocial Personality Disorder
According to the DSM-5, there are four diagnostic criterion, of which Criterion A has seven sub-features.
A. Disregard for and violation of others rights since age 15, as indicated by one of the seven sub features:
- Failure to obey laws and norms by engaging in behavior which results in criminal arrest, or would warrant criminal arrest
- Lying, deception, and manipulation, for profit or self-amusement,
- Impulsive behavior
- Irritability and aggression, manifested as frequently assaults others, or engages in fighting
- Blatantly disregards safety of self and others,
- A pattern of irresponsibility and
- Lack of remorse for actions (American Psychiatric Association, 2013)
The other diagnostic Criterion are:
B. The person is at least age 18,
C. Conduct disorder was present by history before age 15
D. and the antisocial behavior does not occur in the context of schizophrenia or bipolar disorder (American Psychiatric Association, 2013)
Onset
The DSM-5 notes that Antisocial Personality Disorder cannot be diagnosed before age 18, so while an adolescent may display antisocial features, prior to age 18, if diagnostic criteria are met, the appropriate diagnosis would be Conduct Disorder (American Psychiatric Association, 2013).
Prevalence
According to the DSM-5, the annual prevalence of Antisocial Personality Disorder is .02% to 3.3.% when the criteria from prior DSM editions are applied (American Psychiatric Association, 2013).
Risk Factors
The DSM-5 indicates that risk factors for Antisocial Personality Disorder are having a first degree biological relative with APD, and being a male, (American Psychiatric Association, 2013). If Antisocial Personality Disorder is primarily genetic or a product of social learning and other environmental factors has been widely debated by behavioral scientists. There are indicators that Antisocial Personality Disorder is a result of a genetic predisposition in that the individual is born without conscience. There is evidence for neuroanatomical differences in antisocials. A rs-fMRI (resting state functional Magnetic Resonance Imaging) study of n=480 adjudicated antisocial offenders showed “uncoupled connections”in areas of the frontal and parietal lobes which are associated with attention, self regulation, the ability to control oneself, and resolve conflicts . It was noted that physiological and anatomical deficits observed in the frontal /parietal areas, as well as the cerebellum, may account for the chronic low arousal, high impulsivity, lack of conscience, callousness, and decision-making problems commonly seen in individuals with APD (Tang, Jiang, Liao, Wang, & Luo, 2013). There is also evidence that environmental factors, such as internalizing messages from antisocial peers or parents are at work in Antisocial Personality Disorder. One possible developmental pathway if there are not appropriate treatment interventions is ODD, or RAD (Reactive Attachment Disorder) , and CD leading to APD.
Comorbidity
The DSM-5 indicates that Antisocial Personality Disorder is comorbid with substance abuse disorder, and other personality disorders (American Psychiatric Association, 2013).
Treatment of Antisocial Personality Disorder
The DSM-5 does not specify treatment options for APD (American Psychiatric Association, 2013).
The consensus is there is very little in the way of effective treatment for Antisocial Personality Disorder. Individuals with APD may have to be contained by the criminal justice system, through some combination of incapacitation (incarceration), supervision and monitoring (parole, probation, or house arrest), or informal monitoring by local law enforcement to contain their harmful behaviors to others to the greatest extent possible. Some research has shown that individuals with APD do feel degrees of empathy suggesting that at the very least some form of training may be possible (Meffer, Gazzola, den Boer, Bartells, 2013). There are also cases of individuals with APD converting to religion and finding strong conviction within themselves to reform and successfully integrate with society ("Confessions of a Christian Psychopath", 2011). The role of religion and spirituality as a possible treatment for APD is not well studied, and future research is warranted.
Incarceration may not be an effective deterrent to the antisocial individual, as those with APD have difficulty learning from mistakes, are rigid in decision making, and are typically unresponsive to punishment (De Brito, Viding, Kumari, Blackwood, and Sheilagh, 2013). A primary reason that individuals with APD are often non responsive to punishment and deterrence is an inner belief system that views constraints and consequences as a rudimentary function of society, a group which they do not see themselves a part of. The antisocial may see themselves as existing above or beyond society, and thus their existence need not be confined to society's limitations and restraints; and on the contrary, those limitations and restraints are best utilized when exploited to the full advantage of the individual. As a result, for many with APD, incarceration may only serve to reinforce their primary belief system and have little effect towards future deterrence.
The DSM- 5 as well as other sources note that individuals with APD may cease behavioral expression of their antisocial belief system in their 40's (American Psychiatric Association, 2013) although this is inconclusive. Other sources argue that antisocials become too emotionally battered from a long term resisting of society and accumulate physical injuries from a lifestyle of neglect of medical and dental care, untended injuries, and drug and alcohol abuse. This eventual emotional depletion may result in the antisocial reducing destructive behavior or criminal activity simply due to being no longer physically capable. But even in this case, the individual will still retain an antisocial belief system in their day to day dealings with others, and may hide their behavior better through practice effects- learning to be more subtle and not draw attention to themselves and risk arrest or other containment. A specific form of CBT (Cognitive Behavioral Therapy) called CSC (Cognitive Self Change) based on Samenow and Yochelson's seminal work with offenders has documented marginal success at modifying the behavior of violent offenders, both antisocial and otherwise (Barbour, 2013; Powell, & Sadler, n.d. ).
Impact on Functioning
Antisocial Personality Disorder will typically have strong impacts on most areas of functioning. According to the DSM-5, persons with APD may face incarceration as a result of their criminal actions, premature death from violence or accidents, or loss of assets or property from reckless spending (American Psychiatric Association, 2013) or civil forfeiture of assets. Divorce, separation, unemployment, financial dependency on state relief sources, homelessness, anxiety, depression, and suicide rates are all elevated in individuals with Antisocial Personality Disorder when compared to the general population (Goldstein, Dawson, Smith, & Grant, 2012). Antisocials also have the potential to cause great harm to those around them, including family, associates, neighbors, and complete strangers, through financial exploitation, theft, emotional abuse, assault, sexual assault, and homicide.
Differential Diagnosis
There are diagnostic rule-outs for the clinician to consider, in the DSM-5, disorders such as schizophrenia and bipolar disorder, as well as substance abuse disorders should be considered. Even very violent offenders may not be sociopaths, but sociopathy should be considered on a continuum, rather than a dichotomy of present or absent.
References:
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders. (5th Edition). Washington, DC.
Barbour, P. (2013). Criminal Thinking: A cognitive- behavioral therapy approach. ATTC. Retrieved March 4, 2014 from http://madcp.dreamhosters.com/sites/default/files/4F_Barbour_Criminal_Thinking.pdf
De Brito, S.A.. Viding,E., Kumari,V., Blackwood, N., Sheilagh (2013) ; Cool and Hot Executive Function Impairments in Violent Offenders with Antisocial Personality Disorder with and without Psychopathy 8(6): e65566. doi:0.1371/journal.pone.0065566 PMCID: PMC3688734
Meffert, Harma, Gazzola, Valeria, den Boer, Johan, Bartels, Arnold, and Keysershttp, Christian (2013) Reduced spontaneous but relatively normal deliberate vicarious representations in psychopathy. Retrieved Nov 2016 from http://brain.oxfordjournals.org/content/136/8/2550
Goldstein, R.B., Dawson, D.A., Smith, S.W., and Grant, B.F. (2012). Antisocial Behavioral Syndromes and Three-Year Quality of Life Outcomes in United States Adults. Acta Psychiatria Scandinavia 126(2): 10.1111/j.1600-0447.2012.01848.x. 2012. doi: 10.1111/j.1600 0447.2012.01848.x PMCID: PMC3837547 NIHMSID: NIHMS523921
Tang, Y., Jiang, W., Liao, J., Wang, W., and Luo, A. (2013). Identifying Individuals with Antisocial Personality Disorder Using Resting-State fMRI. Plos One. doi: 10.1371/journal.pone.0060652 PMCID: PMC3625191
Turvey, B.E. (1995). The Impressions of a Man: An Objective Forensic Guideline toProfiling Violent Serial Sex Offenders. Knowledge Solutions. Retrieved March 7, 2014, from http://www.corpus-delicti.com/impress.html
Poe, E. A. (1846). The Cask of Amontillado. Retrieved March 7, 2014, from http://archive.org/stream/thecaskofamontil01063gut/1063.txt
Powell, T. and Sadler, C. (n.d.). Cognitive-Behavioral Treatment for Inmates: An Outcome Study Castleton State College, Castleton, Vermont Retrieved March 7, 2014, from www.vtfa.com/presentations/cognitive.ppt
Confessions of a Christian Psychopath. (2011, November). Retrieved from https://healingaspd.wordpress.com/2011/11/28/hello-world/
order-dsm--5-301.81-(f60.81)
Above is from: https://www.theravive.com/therapedia/antisocial-personality-disorder-dsm--5-301.7-(f60.2)

















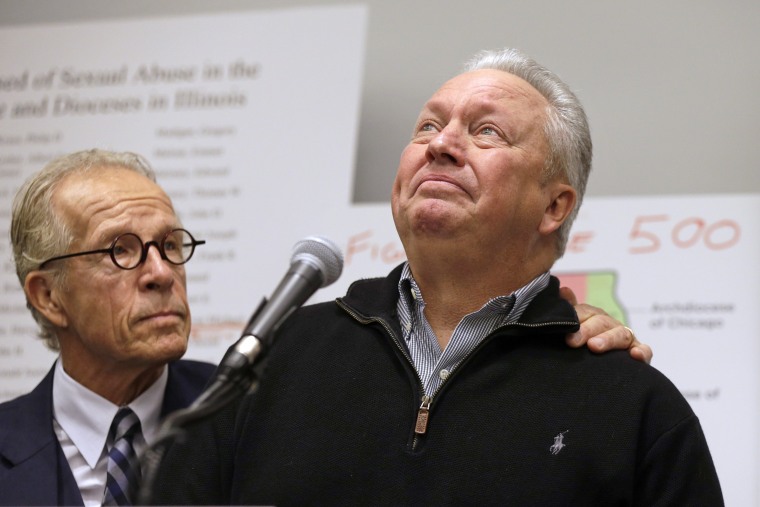 Joe Iacono, right, pauses as he is comforted by attorney Jeff Anderson during a news conference on March 20, 2019, in Chicago.Kiichiro Sato / AP
Joe Iacono, right, pauses as he is comforted by attorney Jeff Anderson during a news conference on March 20, 2019, in Chicago.Kiichiro Sato / AP
